Transcript of Video/Webinar
About the Cellular Medicine Association <–
Charles Runels: Okay, let’s get started. The first question, we’re on the Vampire Breast Lift website, is actually a comment from Wendy Hurn.
Vampire Breast Lift® Questions…
She says, “I have performed several of these procedures to date and have amazing results around six weeks. My own, which is performed nine weeks ago, was amazing. Fullness and firmness with cleavage area many have commented upon. After breastfeeding in the past, I am delighted, so can pass this on to my patients with confidence.”
Thank you very much for writing Wendy.
This is one of those things where it almost seems too good to be true. I’m always grateful when our providers encourage each other. One thing about this when you do these procedures, just be sure you realize there’s a correlation and there’s causation and if you hand out 1,000 Tootsie Rolls to women who walk down the sidewalk, there will be some of them who get breast cancer. If you called it a Breast Lift Tootsie Roll, they might blame it on your Tootsie Roll. I think you can make a very strong argument that PRP is perhaps protective against cancer. We also have the strong research that if you look at the research part of the vampirebreastlift.com.
If you look at the Research tab, you’ll see there’s very good, very strong, research showing that when you mix PRP with fat and transfer it to the breast, there is a trend towards less cancer and there has been two really strong studies showing no increased risk of biopsy or recurrence rate in people who have had breast cancer and then being reconstructed, so it appears to be a very safe thing, but I would still do the same things that you would do for documentation if you were transferring fat to the breast. Most people know you transfer fat to mix it with PRP, so do those same protocols, just make sure the woman has been two things. Make sure seems been recently screened and that whoever keeps track of her breasts says that she’s good to go and number two, make sure you get a good consent form.
Second thing, but hopefully one of you guys will eventually do the research. I think that if you did, if you look at this trend towards less cancer, I think if you did a study where you injected the left breast of a thousand women, you would see a higher rate of breast cancer in the right breast. We don’t know that yet, but that’s what I suspect.
Next one is a question from Dr. Climikoski.
He says, “I have a patient who’s had breast implants and has loss of nipple sensitivity. Her primary concern is to regain the sensitivity back. She asked me, ‘What percentage of people that receive the Vampire Breast Lift do in fact have significant improvement in the sensitivity and are pleased with the results?’ If you provide me with an idea of this percentage, that would be helpful, as I’m a new provider for this procedure and don’t have my experience to draw from. Thank you.”
The answer to this one, I think, is … Again, we don’t have the research. In my practice, it is very near 100%. I’ve actually never had a failure when I was treated someone for loss of sensitivity after implants, but if they had extensive reconstruction, then all bets are off. When I talked to our providers, I hear everything from 50% are improved up to near 100%. I just wouldn’t promise this benefit if it’s for someone for extensive reconstruction, and with everything you do, I highly, highly, highly recommend that you offer a money back guarantee. When I treat this, usually it’s a woman who’s coming for improvement appearance and this is something she wants in addition to that. And so, she’s still happy if her sensitivity isn’t back like she thought it was, maybe, when she was 17. I’ve yet to have a woman tell me it did not make things better than before the procedure.
PRP Science-Techniques (what if the needle clogs?)
Next question is a woman who had … She just wrote this in to me. She says, “I had a 30-year-old,” this came an email but I thought we’d cover it here, she says, “I had a 30-year-old for her O-Shot. We used the Eclipse to spin the blood. My patients PRP was irregular in consistency and had clumps of what I thought had to be platelets. The 27 gauge needle and the syringe, for that matter, clogged a few times. I tried to force out the clumps from the syringe, but I’m wondering why this could’ve happened. Any comments appreciated in advance.”
There’s two things that could be causing clogging. I’ll tell you what they are and I’ll tell you how to deal with this because it can happen to everyone. First, it could be actually the platelet-rich fibrin matrix. I have seen clod up as quickly as two minutes out. This is why when I do this procedure, so in other words when the platelets are in the syringe, just sitting there, they can wait for about six hours in theory and still be okay to use, but once they’re activated; thereby, exposure to thrombin, calcium chloride, calcium gluconate, hyaluronic acid filler, or being excreted from the syringe back into the body exposed to collagen. All those things can cause the platelets to now degranulate, release the growth factors, and then the fluid of the plasma becomes congealed to hold the growth factors in place.
This is called platelet-rich fibrin matrix. It looks like goo inside your syringe. You may want to spend a syringe, activate it, and then just let it sit there and not use it so you can see what this looks like. It looks like little string or a little rubber band or something with a precipitate that forms in the syringe. It’s only probably 10%, 20% of the volume of the syringe will be clotted, but it makes a nice little linear precipitate in the syringe if you just let it sit and congeal. That’s what you’re making.
Now, if there’s turbulence and you’ve activated it can look clotted up in little clumps and that is what you’re seeing if there’s a delay. If you immediately take it out of the centrifuge and you see some little stringy things, maybe that’s platelet-rich fibrin matrix, but I’m not so convinced that sometimes it’s not some of the actual gel itself. I’m told that that’s not the case, but I’m not so clear that what that is and it could be the gel. In any case, I’ve never had it clog the syringe unless I’m slow about getting into the person’s body. When you’re drawing it out, use a … I use a 18-gauge needle to pull it out of the tube and then I have 25-gauge needles, literally within reach, so if I’m sitting there doing the O-Shot or whatever procedure have 25-gauge needles close by. If it starts to gel up and I can’t get it through the needle, then i just grab one of those and swap it out or sometimes you can just swap it before another 27 and whatever matrix is clogged the needle will be stuck in the needle, so when you get a new one, you can keep going. That’s the way to deal with that.
Try to have your patient all the way ready before you ever activate the platelet plasma when you do the O-Shot. Have 25-gauge needles within reach and fresh 27s and you should be okay. Oh, one other thing about the gel. We’ve had a few cases of urticaria. I’ve seen about, well, I’ve seen one myself in the face and I had another man who had some urticaria after Priapus Shot. In both cases, it went away with a Medrol Dose Pack. I’ve had two cases of urticaria reported to me by our providers. One after the face and one after an O-Shot where the woman got some urticaria of the inner thighs. All resolved without sequela using a Medrol Dose Pack.
If you look at the medical literature in some of the orthopedic literature, they talk about this happening and postulate that perhaps there’s a urticaria reaction that some people have to their platelets, but perhaps it’s from the gel itself. I just bring this up as a possibility. I don’t know why it happens, I just know it happens and that’s how you treat it. Maybe some of you guys can help us do that research.
Anything you would add to that Kathleen?
Kathleen Posey: No, but I actually think … I agree with the 25-gauge needle. I actually think I’ve used the 25-gauge needle more so than the 27 because the gel does really get thick and it makes it harder to push.
Charles Runels: So you use the … just routinely use the 25 for the anterior vaginal wall?
Kathleen Posey: Yes.
Charles Runels: While I’m here, just for those who may watch this video because this is all will be recorded and I’ll just post this to where people can see it. This gives a really nice simple diagram about where the material goes. I wonder sometimes if people are using enough. If you use the gel tube, I think you should probably spend three for each side of the breast. The price is set to where you can afford to do that. Basically, 15 milliliters of PRP for each side however you make your PRP. Some of the … I don’t know who knows, but I think some of the people who report not seeing much result are not using enough of this stuff. Let’s see. I think that’s all we had on the breast lift. Let’s look at some of the questions. By the way, anybody on the call who wants to ask a question, just click the raise your hand button and I’ll let you just say what it is you want to ask. Now, we’re on the O-Shot. That was the breast lift. Let’s go down the unanswered questions. By the way, if you ever want to ask a question, this is where to post it. Some of these have gone unanswered, but oftentimes our more experienced people will jump in there and answer a question. This is the way you get more than one opinion.
Priapus Shot® Questions…
Okay, so Dr. Ness has two questions. He uses the EPAT for erectile disfunction, along with PRP, after the fifth treatment and before the sixth. Should we inject PRP more often, say after every treatment? Also, has EPAT been used on women to augment the O-Shot? We’ll do this first question. I actually had an email from one of our urologists this morning. I’m seeing several variations, but most of the variations involve using PRP after the first treatment and after the last treatment, whatever your protocol is.
There was another research paper came out this past July in the Journal of Sexual Medicine showing that this works, but there’s no one that has done, okay, this protocol versus that. We’re still trying to figure this out. There’s a research paper for someone. Obviously, there’s two variables there, how you inject the PRP, or where and when, and how you do whatever physical therapy you’re doing.
More O-Shot® Tips…
I don’t know if anybody has anything to add to that, but the bottom line is that do whatever your normal protocol is, and then do your PRP after the first one and after the last one. Same thing with any sort of these physical therapies, lasers. Whether it’s shockwave therapy or it’s … and your frequency. I know you have the Thermi-Va, Kathleen. When are you adding in Thermi-Va when you do O-Shots?
Kathleen Posey: Well, I add it when they want to have improvement in the labia majora or want to decrease the size of their vagina. What I have noticed consistently now, having done enough of them, I really think when you decrease that distance between the clitoris and the vagina and/or urethra, the orgasms get stronger. I think, I’ve done enough now to know. The patients are telling me now, the ones that have had the Thermi-Va with the O-Shot, that the orgasm has gotten even more intense than the O-Shot, so I think that’s an added bonus.
I wish somebody would do the research to prove that it’s that distance because there’s such a problem when somebody has a baby and things get stretched out AP-wise. What you’re really stretching out is that length between the vagina and the clitoris, and then you’re constantly, as a gynecologist, “I used to be able to have orgasms with penis in vagina. Since I’ve had children, I cannot have orgasms with a penis in vagina.”
I’ve even seen C-section patients that haven’t had a vaginal birth, they’re still stretching out. They still have [inaudible 00:13:19]. They’re still having problems. I think, basically, probably gravity, but they do over somebody’s lifetime take away from your ability to have different types of orgasms.
Charles Runels: When it comes to you, do you do Thermi-Va and then O-Shot immediately following on the first visit, or how do you do your series when you’re combining those two therapies?
Kathleen Posey: Most of the time, I do the O-Shot and the Thermi-Va at the first visit, but sometimes it just depends. If they come in there and just say, “I’m here for the O-Shot,” I do that, and then after I do my exam, and I find they’ve had three kids, and I feel like they could benefit from the Thermi-Va, I give them the pamphlet and talk to them about that. So I’ve done it different ways. I’m not real consistent on … because there’s usually three treatments of Thermi-Va, and I’m not real consistent when I do the O-Shot with it. It can be the third treatment.
Charles Runels: I recently talked to Dr. Alinsod about this too [he does something very similar] and I know, Dr. Posey, you’ve done a lot of these. How long have you been doing O-Shots now, three years?
Kathleen Posey: Four.
Charles Runels: Four, yeah, so you’ve had … and I think probably more than anybody on the planet, your experience with lichen sclerosus combined with PRP is you’ve probably seen more patients than anyone. I don’t say this is for gospel because no one’s done the research, but when I speak to other providers, including Dr. Alinsod, they will sometimes do Thermi-Va, then another Thermi-Va, and then the last one of Thermi-Va, they’ll do Thermi-Va followed by O-Shot, or they’ll do ThermiVa and O-Shot on the first one, and then another Thermi-Va, and then, if they’re doing well, on the last one they just do a Thermi-Va. If they’re not as where they want to be, they’ll add an O-Shot to that last Thermi-Va treatment.
As far as the business part of this goes, a lot of our providers, when they come in, they’ll offer the O-Shot at the regular price, and then if they want to add in the Thermi-Va, they’ll cut the price of the Thermi-Va treatments in half, and sell it all as a package. Anyway, that’s become extremely exciting what people are seeing combining those two.
The general principle though that you never break, I think, is that you don’t do a heat, energy type treatment immediately after the O-Shot or the heat denatures those amino acids, small peptide, chemotactic factors, so you can do them both in the same day, but if you do both, you always just do the O-Shot after the heat therapy. I know you know that Dr. Posey but some of the new people may not.
Kathleen Posey: I have one thing. Can I add one thing
Charles Runels: Yeah, sure. Please do.
HUGE TIP (Small Vagina & Thermi-Va)…
Kathleen Posey: I just treated a patient this week that the Thermi-Va people sent me: Had seen a plastic surgeon in New Orleans, decreased lubrication after chemotherapy for colon cancer. She was in her 40s. No exam. So she gets here, and she’d gone from having intercourse three times a week to barely being even one. It was very, very painful.
Her vagina was so small, and they had done the Thermi-Va, so they were making it smaller, so all her symptoms got worse after the Thermi-Va. Actually, a lot of her pain was in the posterior fourchette. I just treated her this week, but I gave her another shot because I said, “Look, I’m going to see,” but you really have to select the patients and do the exams. If the three of us says, “Okay, I’m going to increase lubrication and decrease pain,” well, if the problem is your vagina’s too small, you’re going to make her worse.
She was worse, so the plastic surgeon complained to Thermi-Va. Thermi-Va says, “Well, where’s her exam?” They go, “Well, I didn’t do one.” They lived in New Orleans, so the plastics doctor called me and said, “Well, will you see her?”
You just really have to take each case individually because she was crippled because of a really small vagina. I don’t know if the O-Shot helped her. I did the traditional O-Shot, and I treated her with pain. I just wanted to throw out all these pain symptoms. I did another one today, which was episiotomy pain, and it’s helped her. She’s a year out and this is her second time. I do do the O-Shot, as well as treat where the pain is.
Charles Runels: Yes, all those are good tips, excellent tips, actually. I’ll just add to that that there probably should be, and maybe you can help us think about this, a … What’s the right word? Sort of a chart where you can picture down the one side is all the therapies, and then across the top are all the different problems, and you pick which do you do? Do you do radiofrequency or laser or PRP or dilators or hormones or whatever? And you can picture a pretty extensive chart.
I agree, not everybody … I don’t even use the word “tight” or “loose” vagina. To me, it’s all about matching your lover, and not everybody needs a smaller vagina, and when it comes to pain, for some reason our O-Shot just seems to be amazing, even when the etiology isn’t always known. But I want to emphasize what you said, if they can put their finger where it hurts, always put a cc of PRP there, and then do the regular O-Shot in addition to that. For example, your lady that had the episiotomy scar. My experience has been that, after an episiotomy, they’re usually good to go. So she lasted a year, and now it’s come back and hurting her again?
Kathleen Posey: Yes, it lasted a year. What she had was an episiotomy scar, and then some scarring around her posterior fourchette as well. It hadn’t come back as bad, but she just said, “I don’t want to have painful intercourse. It worked so well before, just repeat it.” I looked, it was a year ago. That was her second shot.
Charles Runels: Beautiful. That’s encouraging. So it wasn’t all the way like it was, but it wasn’t-
Kathleen Posey: No.
Charles Runels: … it had started to come back. There’s that negative feedback loop that can just make anybody avoid sex, especially, I think, women who have pain, and so breaking that feedback loop is so important. Just anecdotally, another patient I heard about from one of our providers, who’s-
Charles Runels: Just anecdotally, another patient I heard about from one of our providers who stays here with, usually with O-shots, she said she had a lady who had an episiotomy scar that had, not only hurt, but would bleed and tear ’cause the skin was so thin. The tissue was so thin, for years. And, no creams and all sorts of things had been tried with no result. And in this case, it took three injections 8 weeks apart, before the bleeding and the pain was gone. So, 8 weeks, pain’s a little better but not gone. Another one. So a series of three O-shots. So, I’m thinking in some cases the tissue may need more than one procedure.
And then lastly, I know we don’t have it here yet, but I know in Europe they have HA that’s made for the vagina. And then I’m wondering in those cases, it might be helpful to do both. So, like we do with our vampire user HA posteriorly with pure AP on top of it to help build that tissue posteriorly when we have an episiotomy scar. All thought they should not be used anteriorly unless it’s under an IRB protocol because of the risk of granulomas. Okay, let’s do the next question. Anything else you could add to that, Kathleen?
Kathleen Posey: No, that’s fine, thank you.
Charles Runels: Okay, let’s see. So, Cindy Crosby says, “My first question is piggy-backing of a question I read in the previous post. If there are there any post-op instruction pamphlets for vampire clients, please email. Second, I had an O-shot and the client had two large babies with two episiotomies. The anatomies very difficult to maneuver. The urethra’s approximately four centimeters long, it’s in the middle of what appeared to be a build-up of scar tissue. Has anyone experienced this and what was the solution?”
I’m gonna turn this one to you Dr. Posey.
Episiotomy Scars & Pain…
Kathleen Posey: Well, I agree, these can be tough. I would put a red rubber catheter in there and find out exactly where her urethra is. And therefore you would know where to put the PRP. Those are hard because, she probably had a cystocele and if you’re not used to looking at them, you’re not gonna know your anatomy because, it gets very distorted. That’s-
Charles Runels: Mm-hmm (affirmative). So, I think you told me once about a lady who did not get benefit for incontinence and then you brought her back and put in a catheter and then things. Describe for them what you do.
Kathleen Posey: Right, I mean that lady had, I mean you don’t want to say a looser … We have a large vagina had cystocele rectocele I put it where I thought it should be the first time. And she just said it didn’t work and she got on the O-shot website, said my name … This is a long time ago.
Charles Runels: (laughs).
Kathleen Posey: Trust me, okay. She got on and said, “This is horrible.” And I think they gave her a discounted rate. So I brought her in, and I said, “Look, but it didn’t work, you’re going back on.” And she did.
Charles Runels: So you brought her back and repeated it, and she went, and she got better. And so, what you did was put in the catheter? Tell me exactly what you did.
Kathleen Posey: Yeah, I took a small red rubber catheter, you put the other end up on the abdomen, so you don’t get pee everywhere, and then you see exactly how distorted that urethra is, because the urethra is distorted in that patient. And it takes the vagina with it, okay. And so you have to see where to put it. And sometimes it can go off to the left or the right, it isn’t straight in the middle. And that was her problem, it had gone off to the side, and so I just put it in never never land.
Charles Runels: So, in the second procedure, your intention is to put the lumen of the needle in between where the catheter was and the outer service of the vaginal wall? Is that what you did?
Kathleen Posey: Yes, which was probably part of the cystocele and it’s gonna look like it’s scarring, it may not have a normal look by itself.
Charles Runels: Beautiful, very helpful.
Methotrexate…
Okay, let’s see. Dr. Tuttle, “Dear Dr. Runels I have a new person who wants an O-shot, so a daily load dose of methotrexate. Will O-shots still work? Will we get enough PRP, will it work in the presence of this suppressant drug?” She’s using the Emcyte machine.
Okay, so. The general rule I follow is: Would this person recover from surgery? Could you do surgery on them? And if the answer is yes, so can you do it with HIV? Yes. Could you do it with a profound thrombocytopenia? No, not a good idea. So, I don’t know … What’s your thoughts on this one, Kathleen?
Kathleen Posey: I don’t know, but the only P-shot that didn’t work at all was on an 82-year-old with a platelet count of 75,000, and I did two. But I don’t really, I don’t know. I would try it, it’s worth a try. I’d give them money back if it didn’t work.
Charles Runels: Yes, see that’s how I do it. And if you’re new to this, you’re listening to this talk, the first two months, I would just do the easy cases. And of course nothing’s 100% but you have a really high success rate. If not the first shot, the second shot, you’re gonna get it at least 80, 90% of your people well. If you’re treating incontinence with good pelvic floor integrity, dyspareunia, lichen sclerosis, those people are going to get better- people who can have an orgasm but it’s not as strong as it used to be.
If you’re treating someone who’s never had an orgasm in their life, that’s a hard case. Or something like this, where you’re not sure what’s going to happen. I agree, you’re not going to hurt her with this. She would heal, you could operate on her, but is it going to affect this procedure? I don’t know. So this would be a more uncertain case. I would be more hesitant to take these cases until I’ve been doing them. Otherwise, if you do something that’s hard and your first two don’t work, you lose confidence in what you’re doing.
But, on the other hand, I will often take someone who I don’t see any logical reason why I’m doing harm, and then I take them, exactly what you just heard Dr. Posey say, under the condition … I just tell them right off the bat that, “You know, I hope I can get you better. And I’m willing to try this. And if I don’t get you better, I won’t keep your money.” And worst case scenario, you lose a little money but you’ve learned, and you haven’t hurt them, and you’ve helped them find a solution, and you’re still profitable in the next procedure.
Let’s see, I think we just had a question typed in. Okay, yeah, so … Okay, here we go, thank you. So, Dr. Carp I’m gonna unmute your mic, Dr. Carp, so that you can talk with us. Hold on just a second.
Go for it, you there?
Dr. Carp: Yeah, can you hear me?
Charles Runels: Yes sir, perfectly.
Dr. Carp: Yeah, I do all kinds of surgeries on patients with methotrexate, you know, the significance. So I wouldn’t be concerned in the terms of a complication with injecting it. I don’t see how it should have any impact on the expected results with the PRP.
Charles Runels: Beautiful. Thank you for that. When you do your surgery, you don’t anticipate it affecting them healing. So I’m not doing operations every day, so I don’t know that. So, you wouldn’t expect it to have an effect on wound healing. So therefore, we’re both thinking that one variable should not change what the effect of the O-shot would be.
Anything else? Because I know you’ve been doing this awhile, too. Any comments on any of the other questions that we’ve fielded that you want to add to?
Dr. Carp: Not really. I think that, certainly as was pointed out, if they’ve had some uvula-related issues in the rectoceles, et cetera, it does make it more difficult anatomically.
Charles Runels: Mm-hmm (affirmative) yeah. I think it’s never an embarrassment to turf … I love that we have a gynecologists and a urologists as part of our group. And to those in our group who are not, if they see someone where the anatomy is not what you’re used to seeing, I would feel free to … You know, I’ve referred people to Dr. Posey, she’s about two and a half hours from me. And people that … For example, when the clitoris is phymosed down, that’s not something I should be tackling. And so, I send them her to a gynecologists.
And so I encourage those in our group to look at the others in the group that are close to you, so that we can work together.
Let’s see, there’s another. We’ve covered breast lift, the O-shot, there’s some questions that have accumulated about the priapus shot. Let’s go through some of these. Let’s see, okay.
“I was just wondering, can you freeze PRP and then thaw it later before activator procedure? We did a P-shot today, we used pure spin, which do about 20 CCs, and we used 10 of it, so we had some left over and didn’t want to throw it away.”
I know some of the ophthalmologists are putting in the fridge and using it for eyedrops for dry eyes, and using it for a couple weeks at a time. Maybe the answer to this is yes, but I wouldn’t want PRP that had been frozen … You know there’s enough profit built into our procedure that you could afford to spend a kit later. If you wanted, what I would say instead of this is that, there are those in our group that, when they use a priapus shot are using more material.
The only reason these volumes came about is back when I started doing these procedures, back in early 2010, so eight years ago, a one tube of Selphyl, which is what I was using at the time… so, my cost of goods was pretty high. So it was based on what I could find, the amount that could spread through a penis, and I found 10 was what it took to actually infiltrate the entire corpus cavernosoum of an average-sized man.
But others in our groups are using more, so I would say instead of wasting it, just double the volumes and use the whole 20 CCs if he’s average size or larger, and you should get a result. The only place I would say not do that, between the O-shot and the P-shot, is absolutely do not do that with the anterior vaginal wall because, I know of three cases now where our providers got a little overzealous and had an overflow obstruction. It went away and the person winded up doing well, and good results for their stress incontinence, but they went from stress incontinence to an overflow obstruction to wear a diaper for three or four days because of too much volume.
I think anything more than 4 or 5 CCs in the anterior vaginal wall is probably too much. But in the penis, go for it.
Anybody want to add something to that?
Lichen Sclerosus in the Penis…
Okay, so Dr. Leonardo says, “How do you treat lichen sclerosis on the glands? The video does not address this. Do you perform the same injections with the P-shot or would you micro-needle it?”
You know, Kathleen you’re treating a lot of lichen in the labia and around the clitoris, what’s your … This is just a larger clitoris, right? Or you could say clitoris is a smaller penis. What would you say? How would you answer this?
Kathleen Posey: I would inject it right in the areas of the lichen sclerosis, wherever they may be.
Charles Runels: Yep. I would too. I would feel … In a normal priapus shot, you would just kind of … I imagine the glands of the penis, literally like a sponge, and of course the underside of it that’s connected to it is the corpus spongiosum, so it does behave like a sponge.
But I agree with you, if there’s a sclerotic area that you can see or the patient can feel subjectively and put their finger on. I would go intradermally, as best you can, into the sclerotic area and treat it like you would sclerosis anywhere else.
I think, again, we just put out the first paper, I guess it was a couple years ago, and this last paper in the American Academy of Dermatology in January of this year. It’s not like we have some huge body of literature about the best way to do this. It’s part of the reason I like these calls because there’s smart people in this call, and you guys can help us figure out what the best way is. But that’s my best idea for now.
Anybody have anything else? Okay.
Penile Implants…
“I have a patient who has IPP. What is the injection recommendations, techniques, for lidocaine? PRP amounts of each … Locations along the shaft and the depth … In addition, has cold syndrome, for numerous reasons …” whatever.
Okay, so there’s a link here that takes you to a recording when it comes to the penile implants. That, when I interviewed Dr. Joe Banno, who’s one of the urologists in our group … And the biggest thing that I would say here is two things.
I would not use the vacuum pump, and I would not try to inject the shaft at all. And I would consider long and hard whether to even do it at all. Because if their implant fractures that night when they have sex, you could be blamed for it.
But if you do this, and Dr. Banno and I would do this, and most of our providers would do this … I would keep it just to the glands, and come in laterally like you do with the regular P-shot with just the bevel going into the carona of the glands. And just infiltrate the glands, and let that be it. Nothing else, or I think it’s too risky.
Anybody want to add anything to that?
Anyway, watch this video for more details. It’s only five minutes but you’ll get it straight from one of the urologists in our group who teaches. By the way, Dr. Banno teaches urologists how to do implants. It is his specialty. And he has told me that he started making the priapus shot as part of his pre-op before he does the implant because he’s getting more rapid healing and better results, as far as that sensation, and not having that cold feeling.
Any other questions? I think that might be the last one that was turned in. I know we’re only 38 minutes in, but I didn’t come here to try to teach anybody anything. I’m just trying to give us a forum. And our intention is to do this every week because the questions accumulate. And that way, someone other than myself can help think about them.
Anybody on the call have anything else to say or question to ask? Because now is the time and I’ll unmute you and we’ll have it out here for people to comment on.
And I’ll post this video, so who knows? Maybe some other people in our group … We’re pushing 2,000 members now in 40-something countries. We’ve got so many specialties and multiple medical schools, lot of smart people just like you guys are. So, maybe we can get other questions or other ideas.
But anybody have any other questions?
Okay, well I’m on stand-by and I hope this was helpful. And I’ll post the video, and we’ll try to do this every week. So if there’s something that comes in between, this will be the place to get it answered.
Honored to help out, and you guys have a good week. Bye-bye.
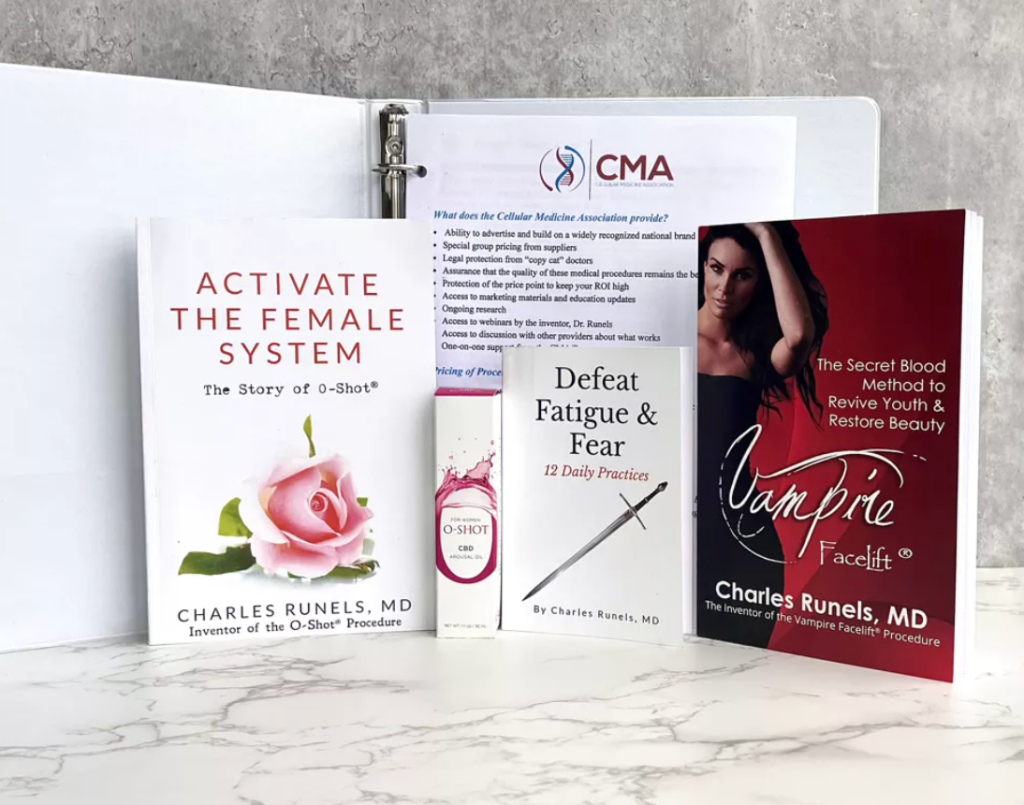
Cellular Medicine Association (CMA). Who we are <–

It’s great to see ongoing research and discussion around the effectiveness of PRP and the P-Shot® for men’s sexual health,…