|
Journal Club with Pearls & Marketing 2024.12.17 Cellular Medicine Association |
JCPM2024.12.17
The following is an edited transcript of the Journal Club with Pearls & Marketing (JCPM) of December 17, 2024, with Charles Runels, MD.
-> The pdf transcript of this live journal club can be read or downloaded here <-<
Topics Covered
- The Warning That Bothered Me Most
- Should You Treat for Free When You’re Not Sure If Your Patient Will Find Healing?
- What to Do (Other Than Surgery) When PDE5is Quit Working
- PRP Attacks Breast Cancer
- Question: PRP for the Buttocks?
- A 100-Year-Old Perspective on Depression and What We Can Learn from Sailors
- References
- Useful Links

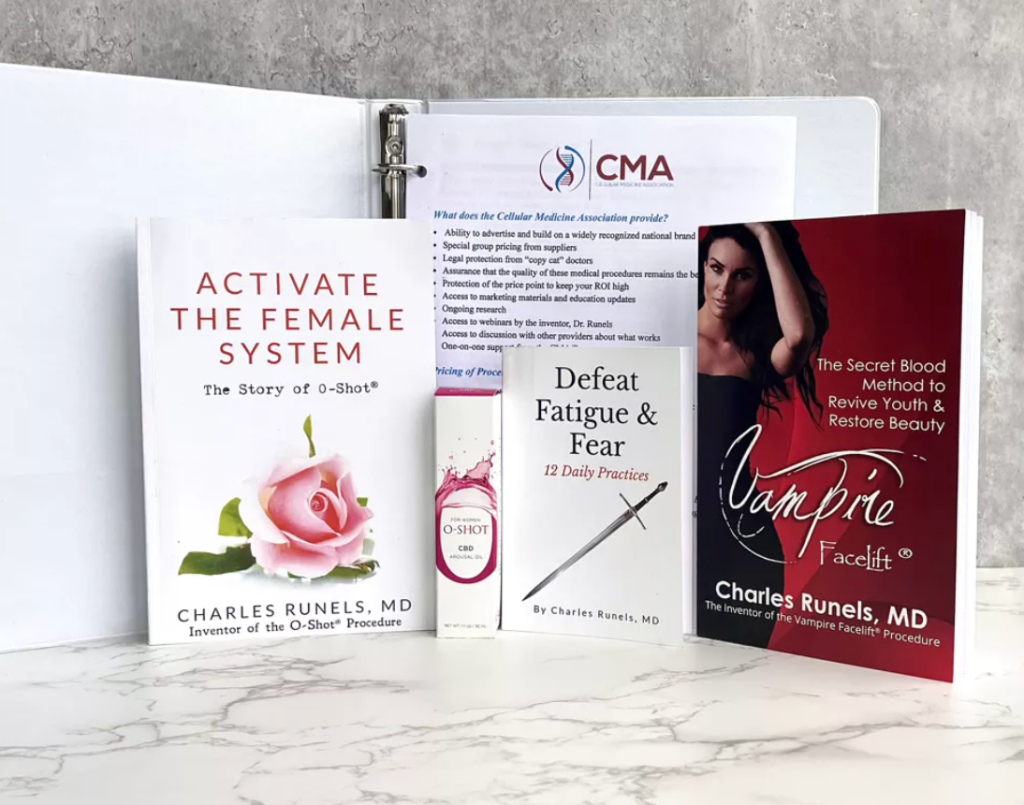
Charles Runels, MD
Author, researcher, and inventor of the Vampire Facelift®, Orchid Shot® (O-Shot®), Priapus Shot® (P-Shot®), Priapus Toxin®, Vampire Breast Lift®, and Vampire Wing Lift®, & Clitoxin® procedures.
Transcript
The Warning That Bothered Me Most
Welcome to Our Journal Club. We have a paper that came out this past week that’s really extremely important to me. Alabama, where I live, has the second-highest rate of basal cell carcinoma in the world compared to every other state and every other country. The last I read, Australia had the highest rate of skin cancer, with lots of blue-eyed people in the hot sun, which is what we have in Alabama as well. As some of you may know, I not only was a lifeguard for seven summers (in Alabama), but I had x-ray treatment to my face back in the ’70s when they treated cystic acne with x-rays. So I’m guaranteed to have basal cells, and I do, and I’ve had multiple surgeries. More importantly, in relation to our procedures, in the beginning, some of the kits, the PRP kits even had on there, “Don’t use it if someone has a history of skin cancer.”
If you were forbidden from using platelet-rich plasma with anyone who just had a history of skin cancer in Alabama, you would be left with not many patients over the age of 45 or 50 years old.
But that’s always been in the back of my mind. What happens if you treat an area that was biopsied?
For example, I had a woman who came to me; she was literally a beauty queen in her youth, but when she saw me a few years ago, she was in her 80s and had an upcoming wedding for a granddaughter. Well, in her forehead, she had a basal cell that was so extensive that, after removing it, they had to do a skin graft, which left this defect in her forehead that was covered by skin. Still, it was a depressed area that covered an oval shape that was probably somewhere around a third of her forehead. You know you can’t put fillers there, even in a normal forehead, because you risk necrosis.
What do you do?
And this is an area that had skin cancer in the past.
I treated it. I treated her on two different occasions, and I did a little mixture where I put a fourth of an HA and three-fourths PRP, and I did a slurry of that and filled it in. We were able to even it out so that she could cover it with makeup.
=>Next Hands-On Workshops with Live Models<=
And I went to the wedding. I also knew the bride and watched the grandmother dance in her pretty dress, proud of her face. But did all that without having research actually knowing what I was hoping. So I’ll get to that paper at the end. But it also relates to, it involves, what about platelet-rich plasma? What does it do to basal cells or squamous cells?
Squamous cell carcinoma, of course, is also important because we’re treating women with Lichen sclerosus who have, I think it’s an 8% to 10% chance of developing squamous cell carcinoma over their lifetime, which is why you want a good biopsy before you treat.
And suppose we’re treating Lichen sclerosus with PRP. In that case, we hope that by decreasing inflammation and decreasing the activity of the disease, we’re also decreasing the incidence of squamous cell carcinoma, just as what is known to happen when you treat the labia with high dose clobetasol in the face of Lichen sclerosus—and now we have research to back up that idea.[1]
But in those who are not responding to clobetasol, what do you do?
Can you use the PRP, or are you increasing the chances of that squamous cell developing? In theory, not. It should be decreasing because you’re decreasing disease activity. But it would be nice to know exactly what PRP does to basal cell and squamous cell cancer cells.
So we’ll get to that, and I’m going to try to come in under 30 minutes again tonight, but I would like to review a couple of papers regarding erectile function. And they’re not so new, but I think they’re helpful.
Hope for Structured Rehabilitation Post Prostatectomy
Let’s pull up this one first. It has to do with rehabilitation post-prostatectomy. A question came up this week. Someone texted me. They have a male patient who had a fractured penis from trauma, and they wanted to know if our P-Shot® procedure would help. No one’s done that study yet, so if you’re looking for low-hanging fruit for a study, there’s your one to do. I’ve had anecdotal reports that it has helped, but it makes sense that it would. The platelet-rich plasma is healing and regenerates healthier tissue, and you have nothing to lose, but you should make it so the patient has nothing to lose, too.
Should You Treat for Free When You’re Not Sure If Your Patient Will Find Healing?
So when I treat someone about whom I’m less certain, I still have them pay me, but I go into it knowing that if they are not delighted with the results, I’ll repeat it once, and if they’re still not delighted, I’ll give them a full refund of their money. And I think that’s how you do that with all of our procedures.
But some people hesitate that if I don’t have as much research to back this up, maybe I should do it for free. We all do things for free, and I recommend that you treat people without charging them when appropriate. Still, I don’t think it’s appropriate to treat them for free just because you’re less certain, but you’re treating them in the face of good scientific reasoning that backs up what you’re doing. Again, you go into it with the understanding that you’re not going to keep their money if they don’t love the results.
But along those same lines, there’s this growing body of evidence about penile rehabilitation. I don’t usually call it erection rehabilitation, but penile rehabilitation post-prostatectomy or post-radioactive seeds. I’ve seen it work in both cases, and we’ve covered this a lot in our Journal Club, but I wanted to go back to some of the earlier papers.
Continuing Penile Rehabilitation
You’ll see this one is from 2016, so almost a decade ago.[2] But the principles here still apply, and I think it’s good to look at the history. It makes me think our reasoning is more solid. So, looking through this as a review, eight years ago. Again, another reason for bringing this up is if you go to the research, there’s still some thread of debate about whether you should even be doing penile rehabilitation. And I think that  comes back to whether you’re going to be a clinician or if you’re just writing philosophical treatises in the literature.
comes back to whether you’re going to be a clinician or if you’re just writing philosophical treatises in the literature.
Because if it’s your penis and you have a marriage and a wife that you love or a lover that you love and you just had prostate surgery, you want everything that might be helpful that isn’t harmful; that’s within reason and makes sense scientifically. So, to me, that’s a moot point as a clinician. It’s like when I used to teach the paramedics back in the ER days. I would teach a few classes for the paramedic course at the local college. And if you remember, the ACLS book has the resuscitation drugs classified. I haven’t upped my ACLS, so I don’t know what it says now, but back then, magnesium was thought to be one of the Class C drugs where it might help, but there’s not as strong of evidence, but not likely to cause harm. Well, I always told my students to tear that out and throw it away because, if your mother’s getting CPR, you want her to get A, B, C, D, F, and G. Every class there isn’t possibly harmful.
And I think I converted a lot of ventricular tachycardia with IV magnesium, and as you know, serum levels don’t correlate well with intracellular levels. It’s a different topic, but the point I’m making is that, as a clinician, it’s not until someone proves it doesn’t work or proves that we’re doing harm there’s enough supportive evidence that you should be offering penile rehabilitation to everyone who has a prostatectomy.
A man that I do business with recently had a prostatectomy at a major university in a big urban area in the United States. He was not offered penile rehabilitation. I don’t get that. I certainly don’t want to think it’s just because the urologist wants to do a penile implant. There’s no way that would be motivation. Maybe they’re also the person who wouldn’t give the Class C drug in the face of CPR, even if it was their mother. I don’t know.
But I want to try everything that might be helpful and not harmful, and going back to these original papers is helpful. And now, of course, we have multiple papers showing that adding in our P-Shot® procedure or PRP in some capacity improves upon this. I’ve put this paper in your handout, and if you go through it quickly, you can see the different classifications.[3] You’ve got trimix or intra-corporeal injections. Then you have, of course, the PDE5 inhibitors and the usual standard procedures, PDE5 inhibitors, daily penis pump every day, or vacuum device every day. But they talk about other things like angiotensin receptor blockers. They even talked about statin therapy. from that one, but they even mentioned a study where statins combined with the PDE5 inhibitors worked better than the PDE5 inhibitors alone. So you’ve got your vacuum pump. Then, I wanted to point out that multiple studies show strong evidence that combining the vacuum device with the PDE5 inhibitor is helpful.[4]
And when they get to the future stuff, they mention stem cells.[5] They don’t mention PRP because six years ago, we weren’t in the literature as much, but the idea of cellular therapies that trigger new tissue, neovascularization, and neurogenesis makes sense. And, of course, now we have those papers about PRP being added in. But I wanted to go back. This is a history.
=>Next Hands-On Workshops with Live Models<=
The strategy is that you’re trying to maintain the pliability of the penis. Even if the man recovers blood flow, if there’s enough delay before recovery happens that the tissue of the penis becomes harder to inflate, it’s like a balloon that you must stretch before you can blow it up. The required pressure to cause erection is greater. So, maintaining blood flow, triggering neovascularization, and maintaining the flexibility of the penis is the strategy behind it.
What to Do (Other Than Surgery) When PDE5is Quit Working
The other one is a history lesson that I think is worth reviewing. I’ve been writing a chapter for another textbook, and that’s why these came to mind: because these are oldies but goodies. This one’s 2018, but they brought up important points that I think are maybe not top of mind that need to be brought top of mind. We have our P-Shot®, and so we’re thinking about that. But it’s useful to go back and look at what did we do before we had that. Because most of that at least still applies. This is a nice review of an article from six years ago about other strategies for the 30% of men that PDE5 inhibitors alone are insufficient.[6]
Now, as you know, I think that our P-Shot® ought to be first-line because, unlike the PDE5 inhibitors, our P-shot reverses or slows or at least has the potential to reverse or slow the progression of the pathophysiology causing erectile dysfunction if there’s a neurovascular disease in the penis itself. And Viagra or the PDE5 inhibitors, nothing, the intra-cavernosal injections, and, of course, penile implants don’t do that. They don’t reverse the pathophysiology. S
Why should you wait until PDE5 inhibitors quit working?
But when you look at what options you have when they stop working or if they’re not tolerated due to headaches, visual changes, or some people’s back pain, then, one, they have strategies. It’s like the 12 commandments: They number them to 12. Switching from one to another, you’ve got this when you can download it, but it really lays it out in a very organized way.
You’ve got to increase the dose above what’s on the label. Combining two, they talk about combining a long-acting with a short-acting, using daily instead of on demand. Of course, replacing testosterone. I don’t know many people who do the alpha-adrenergic antagonists, but that’s an option, combined with the local injections, either brand name or your trimix. Again, I don’t know as many in our group that use the intra-urethral alprostadil, but some do. Then, it can be combined with low-intensity shockwave therapy or a vacuum device. 
Again, we were not as much in the news back when this paper. We were doing it. I first reported the P-Shot to the U.S. Patent and Trademark Office in 2010. This was eight years after we were doing P-Shots, but we had trouble breaking into the literature, and I focused most of my attention on the O-Shot®. So, it’s not mentioned in this paper, although, as I’ve mentioned, we have multiple papers that do now. But these are all things you can do when the Viagra or the Cialis doesn’t work in addition to your P-Shot.
If they’re already on a PDE5 inhibitor and it’s quit working, they will tend to want to stop it to see if the P-Shot will help. But that’s two variables simultaneously. You stopped one medicine, and you started another therapy. So, I have a definite and clear conversation that takes a few minutes. It’s an investment in your time, but I make sure all my male patients know that getting them to their best erection and their best penile health is my primary aim. After that’s achieved, we can start seeing what we can do without. And it’s not as important to me as I’m getting them there to know.
Is it the penis pump?
Is it the PDE5 inhibitor?
Is it the P-Shot?
We can tease that out by stopping one or the other or decreasing dosages later. But the first thing is to get you to where things are functioning the way you want them to. Then, as the regenerative cellular therapies kick in, your penis becomes healthier somewhere around six to eight weeks, when you have your best direction—then consider stopping some of the therapies.
Or maybe you don’t. We repeat it, or we add something else, but I don’t think it’s a good idea to stop your PDE5 inhibitor immediately. Your P-Shot hasn’t even had time to work. Remember, it’s not a pharmacological effect. You must wait for the tissue to grow. The full effect is probably 12 weeks. That’s the way it is in wound care studies, where you must wait for the new blood flow in the new tissue.
So, I have people continue what they’re doing, add in my P-Shot, and add in other things. And you can see somewhere at the beginning it talks about lifestyle changes. As a rule, just a new aerobic exercise routine will bump a man’s erections by five to seven.
PDE5 inhibitors; bump it about the same.
And our P-Shot bumps it about the same, five to seven.
Depending on where a man is starting, he may need all of those therapies to make it to where he wants to go. Now, I have 10 minutes. So, let’s talk about the idea of squamous and basal cell carcinoma. And then, I would love to have your comments and corrections, and we’ll end it with a quote I found in an old textbook written back in the 1800s. But let’s start with this. We mentioned this about two weeks ago. This really warmed my heart.
PRP Attacks Breast Cancer
I think it’s a landmark study because we had indirect evidence that PRP might be somehow decreasing the proliferation of breast cancer because we had the study of the scar from the removal of a port for chemotherapy.[7] And the women in the group that was treated with PRP had less recurrence and less mortality. The women who got saline had four deaths, and in the group that got PRP, there was no death and less recurrence. And the authors were bothered by that. They were trying to show that there was no increase in cancer rates among breast cancer patients, but they didn’t even want to believe their own numbers. It was so revolutionary.
These doctors said, “Well, okay, maybe that’s real.”
They examined in vitro and demonstrated that PRP was a treatment—it killed cancer cells.[8]
I’m calling that a landmark study because no one else has done that paper. And then that’s the only two I know of where someone, the one with the scar and then that in vitro study, that showed breast cancer was possibly at least prevented, if not, in some ways, adjunctively treated. I’m not saying it prevents it completely. Again, I’m saying that in a population,
I’m trying to couch or attenuate my claim here, not to sound like I’ve lost credulity, but it is what it is. PRP in vitro killed breast cancer cells, and more studies need to be done quickly because that’s an important finding.
Now, what these people did was they took the same thing, in vitro, but they call it nonmelanoma skin cancer, and that would be basal cell and squamous cell carcinoma.[9] And then they treated with PRP. I’ve highlighted here for you what I think are the most key ideas.
There are only a few key ideas.
It demonstrated the potential to be at least an adjunctive treatment for basal cell carcinoma. I’ve still got a few wanting to grow on my face. I believe it enough that I’m going to treat my face because I’ve got them in places where I’m not ready to lose another piece of my face. So, it’s worth trying. I’m not saying this needs to be the standard of care, but it should not be ignored.
This is absolutely a landmark study that should be noticed. All right, so they mention here in the paper the regenerative parts, the regenerative properties of, they call it PRF, but as you know, when you activate PRP, it becomes platelet-rich fibrin. And so, here’s the key to the whole paper. I’ve got the reasoning behind it highlighted for you. Hold on a second right here. Pardon me, just let me just read this paragraph.
“Leukocytes, including neutrophils and monocytes, play crucial roles in inflammatory response by contributing to the removal of pathogens and modulating immune reactions. Neutrophils acting as the first line of defense against infections exhibit selective cytotoxicity against tumor cells in vitro, potentially by releasing reactive oxygen species and proteolytic enzymes. Recent studies have highlighted the continuous release of growth factors in cytokines from liquid PRF.”
They list the factors there: “tumor growth factor beta one, vaso endo growth factor, endothelial growth factor, crucial, various cascades of angiogenesis regeneration and wound healing.”
This is what I was getting to. “Platelet-neutrophil interactions enhance the oxidative burst, promote neutrophil extracellular trap formation, and enhance phagocytosis, which is critical for host defense mechanisms. The cytotoxic effects of human platelets on tumor cells have already been observed in vitro.”
So I mean, there’s more there, but to me, that’s the key of what they showed, which is that, at least in vitro, basal cell carcinoma and squamous cell carcinoma do not like PRP. And, again, I don’t think that means you go squirt every basal cell you see. To me, Mohs surgery is the definitive therapy for it. But if it’s in a place that’s hard to get to or possibly deforming, maybe this isn’t something to try before you chop off a nose, an ear, or a big piece of somebody’s mouth. At the very least, I think it’s reassuring that when we treat Lichen sclerosus patients, if there’s a dormant squamous cell carcinoma, perhaps we’re actually preventing the conversion or attenuating the growth of that squamous cell carcinoma.
It is reassuring to me just to be able to say, “Perhaps that is the case from this study.”
So, yay for these investigators. This just came out. It truly came out in January. So, I think this is a truly landmark study.
Question: PRP for the Buttocks?
So, I put a YouTube video out there for PRP injections for the gluteal region for fat growth. Treat the lower curve of the buttocks. It’s an upside-down heart with those two curves at the bottom.
You fill them with PRP like you would the cleavage of the breast with at least 15 milliliters per side, which means you’ll have to spend at least 60 milliliters of blood. And you inject it into the fat.
I came across something in an old book today that I thought was worth remembering. Let’s see if I can show it to you, and then we can call it a night.
A 100-Year-Old Perspective on Depression and What We Can Learn from Sailors
Okay, here we go. This is from a book that came out in, I think, 1878. It’s Insanity: Ancient and Modern Life with Chapters on its Prevention. This guy was a famous psychiatrist and physician back in London over 100 years ago. But I thought he had a couple of things that were worth remembering. I mean, this is so old. He thought he was only postulating that perhaps when you have incest, that would lead to people not being so smart.
They just mostly had observation. But this was, I think, worth remembering as you see people, young people do stupid things on the news twice in the past couple of weeks, just tragic, stupid things. He calls it out.
He says, “Alarm should be felt when the young seek solitude and society is carefully shunned. The excessive cultivation of the imagination, castle building, and the absorption of the mind and works of fiction are highly detrimental to the mind’s health.”
And seeing what happened in New York with the CEO being shot and the guy disappeared and just went missing to his family for a while. And, of course, we had COVID, and all of our children were isolated for too long, and all the mental health problems that came from that. But I think it’s a good reminder that, before they had more sophisticated ways of thinking, and when you see a young person withdraw from society, it’s a warning.
And then this one, and then I’ll stop. He says, “Attack the first symptoms of mental ill health by appropriate means with at least as much determination as the first threatening of consumption or gout or bronchitis. Repel the invader before he can plant his foot firmly on your,” and I’ll leave it to your imagination what’s on the next page.
They didn’t have pharmacology back then. A change of scenery, and he talks about diet. He talks about and makes a good case for depression in Roman times, Egyptian times, and the Israelites 2,000 years ago, as well as how it manifested and was talked about in some of the ancient writings. And it was there. But what he said is you don’t see is you don’t see depression in sailors on a ship because a sailor on a ship does not have the luxury of thinking about anything but immediate present moment. Because if your mind wanders, you could die. And I think that’s why, as an ER doctor, many of you as surgeons, when you’re at work, you’re at peace because your mind has to be on the present moment as you place a stitch or you have a scalpel in your hand or someone’s bleeding out.
And so, in some ways, modern civilization propagates mental illness,
We have much fewer beds in the U.S. per population than what’s seen in, say, Switzerland and London, as well as other countries. So, I’m hoping that gets better.
But anyway, I thought that might be of interest to you, and I hope you have a good night. I think the takeaway is that if you want to use this as a lesson that brings people to your office, I would write a little note about penile rehabilitation and put a link to that paper I gave you and say, “You don’t have to wait until you have prostate surgery. You don’t wait until you have a stroke to lift weights. We can rehabilitate your penis from where it is now to a healthier state, a more functional state. Use the pump now. Use our P-Shot now.”
As you know, low daily doses of Cialis can help the prostate. There’s one paper that shows it decreases the incidence of dementia. So we can do some stuff now instead of waiting until the pathology. Adding an email to that effect with a link to that paper would bring new patients. And those of you who are doing the O-Shot for Lichen sclerosus, now you have, I think, some reassurance that that’s okay. Hopefully, this will progress over the next few years, and we’ll have more research showing us, hopefully, actually treating basal cells, at least partly, with PRP. I don’t think it’s time to say that’s what we do, but today’s paper I think was the landmark encouragement in that direction. Okay, you guys have a great night. I hope that was helpful for you.
=>Next Hands-On Workshops with Live Models<=
References
Dohle, Eva, Lianna Zhu, Robert Sader, and Shahram Ghanaati. “Effect of Liquid Blood Concentrates on Cell Proliferation and Cell Cycle- and Apoptosis-Related Gene Expressions in Nonmelanoma Skin Cancer Cells: A Comparative In Vitro Study.” International Journal of Molecular Sciences 25, no. 23 (January 2024): 12983. https://doi.org/10.3390/ijms252312983.
Eichler, Christian, Jens Üner, Fabinshy Thangarajah, Julia Radosa, Max Zinser, Lotta Ada Fischer, Julian Puppe, Matthias Warm, Wolfram Malter, and Caroline Lenz. “Platelet-Rich Plasma (PRP) in Oncological Patients: Long-Term Oncological Outcome Analysis of the Treatment of Subcutaneous Venous Access Device Scars in 89 Breast Cancer Patients.” Archives of Gynecology and Obstetrics, April 4, 2022. https://doi.org/10.1007/s00404-022-06416-4.
Han, Chao, Caiping Chen, Ning Lu, Li Xue, Dan Xing, Wanxin Wu, Wang Li, and Xiang Lu. “Platelet-Rich Plasma Inhibits Breast Cancer Proliferation.” Clinical Medicine Insights: Oncology 18 (January 2024): 11795549241298978. https://doi.org/10.1177/11795549241298978.
Lee, Mary, and Roohollah Sharifi. “Non-Invasive Management Options for Erectile Dysfunction When a Phosphodiesterase Type 5 Inhibitor Fails.” Drugs & Aging 35, no. 3 (March 2018): 175–87. https://doi.org/10.1007/s40266-018-0528-4.
Sopko, Nikolai A, and Arthur L Burnett. “Erection Rehabilitation Following Prostatectomy [Mdash] Current Strategies and Future Directions.” Nat Rev Urol 13, no. 4 (April 2016): 216–25. http://dx.doi.org/10.1038/nrurol.2016.47.
Tags
Journal Club, PRP, basal cell carcinoma, squamous cell carcinoma, skin cancer, Alabama, Lichen sclerosus, platelet-rich plasma, erectile dysfunction, penile rehabilitation, prostatectomy, P-Shot®, vacuum device, PRF, oncology, penile health, regenerative medicine, in vitro study, penile implants, penile health, cancer research, neovascularization, PRP therapy, gluteal region, fat growth, mental health, historical medicine, lifestyle changes, Charles Runels
Helpful Links
=> Next Hands-On Workshops with Live Models <=
=> Dr. Runels Botulinum Blastoff Course <=
=> The Cellular Medicine Association (who we are) <=
=> Apply for Online Training for Multiple PRP Procedures <=
=> FSFI Online Administrator and Calculator <=
=> 5-Notes Expert System for Doctors <=
=> Help with Logging into Membership Websites <=
=> The software I use to send emails: ONTRAPORT (free trial) <=
=> Sell O-Shot® products: You make 10% with links you place; shipped by the manufacturer), this explains and here’s where to apply <=
|
Charles Runels, MD 888-920-5311 CellularMedicineAssociation.org |
Page of |
[1] Dohle et al., “Effect of Liquid Blood Concentrates on Cell Proliferation and Cell Cycle- and Apoptosis-Related Gene Expressions in Nonmelanoma Skin Cancer Cells.”
[2] Sopko and Burnett, “Erection Rehabilitation Following Prostatectomy [Mdash] Current Strategies and Future Directions.”
[3] Lee and Sharifi, “Non-Invasive Management Options for Erectile Dysfunction When a Phosphodiesterase Type 5 Inhibitor Fails.”
[4] Lee and Sharifi.
[5] Sopko and Burnett, “Erection Rehabilitation Following Prostatectomy [Mdash] Current Strategies and Future Directions.”
[6] Lee and Sharifi, “Non-Invasive Management Options for Erectile Dysfunction When a Phosphodiesterase Type 5 Inhibitor Fails.”
[7] Eichler et al., “Platelet-Rich Plasma (PRP) in Oncological Patients.”
[8] Han et al., “Platelet-Rich Plasma Inhibits Breast Cancer Proliferation.”
[9] Dohle et al., “Effect of Liquid Blood Concentrates on Cell Proliferation and Cell Cycle- and Apoptosis-Related Gene Expressions in Nonmelanoma Skin Cancer Cells.”

It’s great to see ongoing research and discussion around the effectiveness of PRP and the P-Shot® for men’s sexual health,…