|
Journal Club with Pearls & Marketing 2024.11.26 Cellular Medicine Association |
JCPM2024.11.26
The following is an edited transcript of the Journal Club with Pearls & Marketing (JCPM) of November 16, 2024, with Charles Runels, MD.
>-> The PDF of the transcript of this live journal club can be seen here <-<
Topics Covered
- Relevant History of Fat to the Breast
- Afraid to Believe the Math
- How Could PRP Prevent Breast Cancer?
- A Look Back to Remember to be Humble
- PRP as a Treatment and Prevention of Breast Cancer?
- O-Shot® for Dyspareunia Post Breast Cancer
- References
- Helpful Links

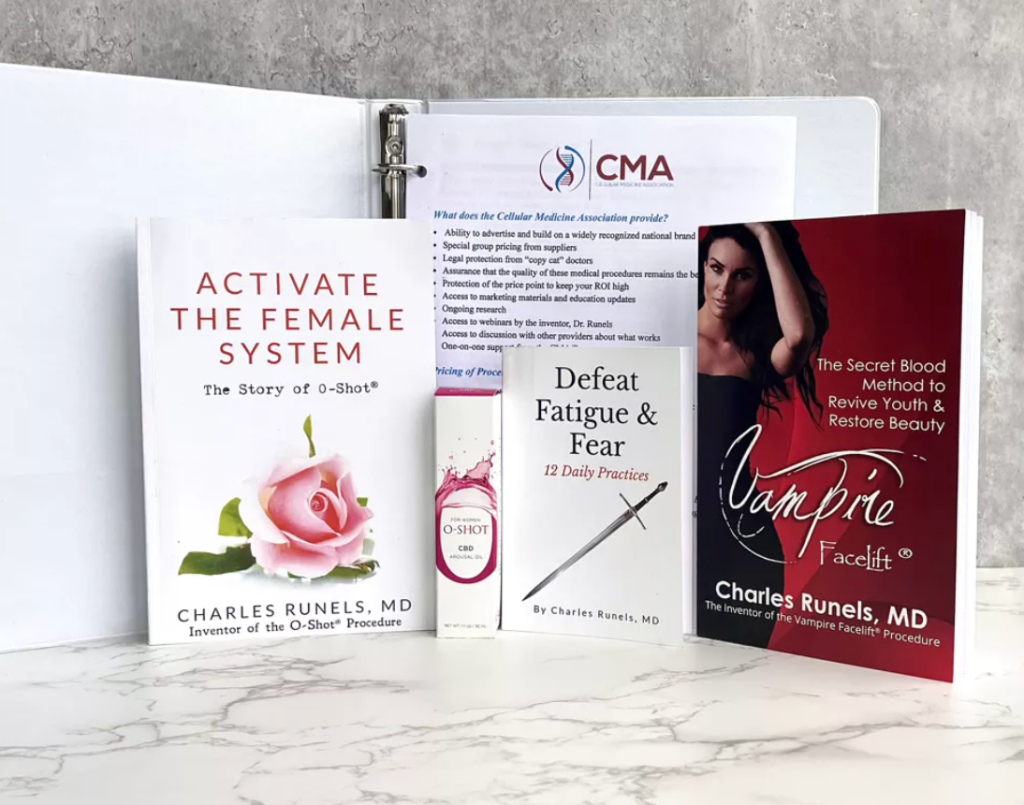
Charles Runels, MD
Author, researcher, and inventor of the Vampire Facelift®, Orchid Shot® (O-Shot®), Priapus Shot® (P-Shot®), Priapus Toxin®, Vampire Breast Lift®, and Vampire Wing Lift®, & Clitoxin® procedures.
Transcript
Relevant History of Fat to the Breast
I’m very excited about the Journal Club tonight. I’ve been looking for a paper like this. I didn’t think I would ever see it. I thought we would have to do it. We’ve been doing our Vampire Breast Lift®[1] for over a decade. In thinking about the safety of that procedure, we have leaned mostly upon three studies looking at the safety of fat grafting to the breast.[2] [3]
That’s been done now for close to two decades. When they surveyed plastic surgeons, somewhere around 80% of plastic surgeons do fat transfer to the breast,[4] usually mixed with platelet-rich plasma (to increase survival of the fat)[5] and often done post-mastectomy. So, three different studies were done. This is one of them, looking at what happens to the incidence of breast cancer after fat transfer to the breast. In all the studies, there was no statistical difference between women who had fat transferred and those who did not when they looked at re-biopsy rates and recurrence rates.[6] [7] [8]
But that’s a little bit of a workaround.
The metaphor was if the spaghetti was safe, then the sauce without the noodles was safe. Usually, the fat is mixed with some PRP, so if both are safe, then the PRP alone should be safe. However, we didn’t have much direct research with PRP alone.
Then, a couple of excellent papers came out. One was this one where they looked at using PRP to inject around where the biopsies were taken, and then there was an actual decrease in the recurrence rate.[9]
And I put this paper in your download box. I’m getting to the one that just came out.
And then, this one really excited me because, with this one, which has been out now for several years (it came out in 2022) they looked at women who had had the port taken out (placed for chemotherapy), and now you’re left with a scar, and they injected the- because PRP helps with scarring.[10]
And then they followed to see what would happen.
Afraid to Believe the Math
This was the only time I’ve seen this happen in a research paper. Statistically, those who had the PRP for the port did better. There were no deaths in the group that had their port scar treated with PRP, and there were four deaths in the ones who did not have the PRP.
There was also a statistical difference in recurrence rates (PRP-treated women had fewer recurrences).
And so, the conclusion was that it appeared safe, but they couldn’t bring themselves to say “it.”
I’ve never seen this in another paper, and even though it is statistically significant, they hedged their bet. Essentially, they did this revolutionary study, then wimped out and said, “Even though we’ve got the stats to prove it, we still think it’s a coincidence [that women treated with PRP had less recurrence of their breast cancer and increased survival]. And we do not think that PRP actually decreased the incidence.”
Safe to say, but in conflict with their own study. Who does that?
But, I understand: it would be very bold for them to say, “We’re preventing breast cancer with PRP.”
That would be bold, but I had to chuckle when I realized they were afraid to say it even though the math demonstrated it.
How Could PRP Prevent Breast Cancer?
But you’re still left wondering why or how.
So I leaned back on this study, and again, I put this one in your download section; that is my theory, and it turns out I’m probably wrong about this, at least in some cases, a theory had to do with this. You think, “Well, how could growth factors cause less cancer?”
And in this study, Canadian doctor, this has been out, I think, maybe 10 years now. In this study, a man and his colleagues cultured the breast, and they found a different microbiome. They hypothesized that perhaps there’s more inflammation, and somehow, the different bacterial milieu in the breast that developed cancer was different than the healthier breast.[11]
At least, that’s what they demonstrated.
=>Next Hands-On Workshops with Live Models<=
And maybe it was causative and not correlative. So that was my theory was that maybe that’s why the PRP is helping since we know it’s antibacterial. Maybe the PRP is changing the bacterial milieu to a healthier state, more like the non-cancerous breasts, or perhaps decreasing the recurrence rate, which would be at least a hypothesis for why in these studies of no biopsy injections and injection around the scar of the port that was removed or the scar of the breast from where the port was removed, might decrease the cancer rate.
And that was all I had to run with.
Now, before I show you the new paper that came out, another conflict in reasoning or counterintuitive idea, some of you know I did some phase four clinical trials with Genotropin® about 20 years ago and with Seizen®. I was involved in growth hormone research. 
I was very involved, and I read everything ever written about growth hormone replacement in adults—all of it.
And there was a study in children who had pituitary tumors.
Now think about the quandary you’re in if you surgically remove a brain tumor from a child and your surgery now has goofed up their production of growth hormone, and it’s a child, yet you just removed a cancer.
Do you give them growth hormone to help their development and risk possible recurrence of the cancer?
Or do you not give them growth hormone for fear of that and let them not develop as normally as they would?
Well, they divided the group in half, and the children who got the growth hormone developed better or more in line with their age and had fewer recurrences of the pituitary tumor.
So I can’t explain that. I know that was a study that was done.
And so I’m still left in this quandary (less cancer with growth hormones).
And then we got this paper, which I’m very excited about, that came out recently in the past couple of weeks.
A Look Back to Remember to be Humble
And I’ll show it to you. And I’m going to leave you hanging, though, because otherwise I’ll forget.
I want to show you this. I bumped into this this past week. This is one of those well-read Geriatrics back textbooks published in the 80s.[12]
And I want you to look at this paragraph, “Most cases of secondary impotency…” And they’re defining that as the man was able to get an erection and then developed impotence versus never having an erection in his life would be primary. “Most of them are psychogenic.”
And they give you, look at that, five different references to back it up about why.
And Dr. Finkle is the one writing it. I’ve read quite a bit of his stuff because Finkle wrote the article that motivated me to plunge into the PRP and Priapus, the whole Priapus Shot® idea.
But he was advising psychotherapy for ED for 85% of men in this Geriatric textbook.
So this is not a one-off throwaway journal.
This is the accepted dogma of the early 1980s.
Imagine the frustration of the man who’s trying to be psychotherapy into having an erection when he truly has neurovascular disease as the etiology.
This is useful to look at, in my opinion, (not to criticize Dr. Finkle), because now I think, “Well, what am I getting wrong?”
Now, it’s easy to point fingers back four decades; I was 23 in 1983. I’m 64 now. So that’s easy to point back and say, “Ha ha.”
But the real question is, what are we getting wrong now?
What are we missing?
Or what are we seeing that maybe our colleagues are missing?
That’s the real thing. It’s easy to point backward, but I want to make sure you got it—I do not claim to know the answers.
I have more questions than answers,
I think. But I hope there’s going to be a plethora of research because of what I’m about to show you.
PRP as a Treatment and Prevention of Breast Cancer?
Okay, so this one just blew me away. They looked at in vitro and in rats. I’ll just read this to you. They first bring up the question I just talked about: PRP. It’s nice to treat scarring and reconstruction with. They quote some studies I just told you about, such as the subcutaneous venous access device.
They’re quoting that study I just quoted, and they actually went and looked at it in more depth. Thank goodness, I haven’t gotten around to it yet, nor has anybody else I know of. I love these guys and I’ve never met them. Thank you.
Some of you know I lost a sister to breast cancer. I hate breast cancer. So, 45 months out, and there was no cancer recurrence in the scar tissue where they injected.
So these guys said, “Well, okay, let’s look at it.”
So they used in vitro, and they had mice where they implanted cells to have a model of breast cancer.
=>Next Hands-On Workshops with Live Models<=
And then one group had PRP injected around the cancer, and the other group got saline injected around the cancer, which, as you guys know, I don’t think it’s really a placebo.[13] [14] You do get some hydrodissection, and there’s some effect. But they used saline as a placebo; then they sacrificed the animals.
And look at the conclusions!
PRP inhibits the growth of breast cancer in mice.
It inhibits the breast cancer proliferation.
It promotes apoptosis.
It’s the bomb.
So I don’t know what to do with this yet, but at the very least, it makes me feel even better about our Vampire Breast Lift® procedure.
I’ve always told people that when we do our Vampire Breast Lift®, you do the exact same things you would do if you were doing fat transfer to the breast: you must make sure the woman has had a recent exam and or mammogram if that’s what she and her doctor are doing. And then you get a good consent form. Since one in eight women get breast cancer, if you had a lollipop, you called the breast enhancing lollipop, and you give it out to enough women. Eventually, one in eight is going to get breast cancer—and you do not want it blamed on your lollipop.
But if the inclinations are that by multiple studies now over the past two decades that we’re not proliferating some occult cancer, we could actually be indirectly by those two studies of the node biopsies and treating the scar tissue left by the port; there was an inclination that we might be preventing, or not preventing, but decreasing the chances of recurrence in a population (not guaranteeing it wouldn’t occur and reoccur in one individual woman).
I’m so glad these people did this study.


This is a landmark study: They showed platelet-rich plasma in vitro and in mice shuts down breast cancer. That’s a revolutionary idea.
I think the next thing needs to be a population study where you take women who’ve had no cancer and you inject 500 women, you inject all their left breasts, and you watch them for 40 years to see if they get more cancer in the right breast than the left.
And hopefully, you must stop the study at five years because it’s working so well—and go back and inject all the right breasts.
Eventually, I think our grandchildren will have PRP injected into the breast as prophylaxis for breast cancer. I’m not ready to say that now, but this is a crazy good paper that, at the very least, gives us reassurance about our vampire breast lift. And that’s the main thing I have for you guys tonight.
=>Next Hands-On Workshops with Live Models<=
I had one other paper I wanted to show you just because we’re on the subject of breast cancer.
O-Shot® for Dyspareunia Post Breast Cancer
Give me a second. Yes. This study right here that came out in Menopause now, I don’t know, probably seven, eight years ago. Yeah, 2018. So six years ago. And I don’t know why it’s not more talked about, but they showed injecting. This was a Regen kit. They have a kit that comes with HA that’s not FDA-approved yet in the US, but they used a Regen kit that has a non-cross-linked HA injected into the anterior vaginal wall.[15]
And women with breast cancer didn’t want to be on hormones and it was significantly helpful for their dyspareunia secondary to dryness. So I don’t think I’ll put this one in your download box and we put a link to it in the chat box. And then I think with that, I’ll call it a night. I know it’s the holidays. I’m surprised you, I’m happy you guys are here and see some of the true and faithful. So thank you very much for being here. I’m in New York to see my two sons and hopefully see the Macy’s Parade.
I brought my mother up here to see the Macy’s Parade (and visit with my sons), but this was just too good. I had to do it tonight.
So let me put this in the chat box, and then I’ll see if you guys have any questions, and we’ll call it a night. Just a second. Okay. Here’s the link to that menopausal-breast-cancer study;. We all know someone who’s had breast cancer, right?
And many of them many of your patients have had breast cancer, and they may not know you have something better than KY Jelly to help them with the dyspareunia secondary to breast cancer with no estrogen post-therapy.
Nope, no questions.
I put it to my patients by having them sign the consent form and saying, “I don’t know. I hate breast cancer. I don’t in by any means think that I’m giving you a vaccine against breast cancer, but I have hopes that when we do this Vampire Breast Lift®, we’re decreasing your chances of it occurring.”
That could be something based on current research, and I think you have more reasons to say that now.
All right, have a good night. I hope that was helpful.
References
Asghar, Aneela, Zahid Tahir, Aisha Ghias, Usma Iftikhar, and Tahir Jameel Ahmad. “Efficacy and Safety of Intralesional Normal Saline in Atrophic Acne Scars.” Annals of King Edward Medical University 25, no. 2 (June 24, 2019). https://doi.org/10.21649/akemu.v25i2.2867.
Eichler, C., C. Baucks, J. Üner, C. Pahmeyer, D. Ratiu, B. Gruettner, W. Malter, and M. Warm. “Platelet-Rich Plasma (PRP) in Breast Cancer Patients: An Application Analysis of 163 Sentinel Lymph Node Biopsies.” Edited by Xin-yuan Guan. BioMed Research International 2020 (October 22, 2020): 1–7. https://doi.org/10.1155/2020/3432987.
Eichler, Christian, Jens Üner, Fabinshy Thangarajah, Julia Radosa, Max Zinser, Lotta Ada Fischer, Julian Puppe, Matthias Warm, Wolfram Malter, and Caroline Lenz. “Platelet-Rich Plasma (PRP) in Oncological Patients: Long-Term Oncological Outcome Analysis of the Treatment of Subcutaneous Venous Access Device Scars in 89 Breast Cancer Patients.” Archives of Gynecology and Obstetrics, April 4, 2022. https://doi.org/10.1007/s00404-022-06416-4.
El-Amawy, Heba Saed, and Sameh Magdy Sarsik. “Saline in Dermatology: A Literature Review.” Journal of Cosmetic Dermatology 20, no. 7 (2021): 2040–51. https://doi.org/10.1111/jocd.13813.
Hersant, Barbara, Mounia SidAhmed-Mezi, Yazid Belkacemi, Franklin Darmon, Sylvie Bastuji-Garin, Gabrielle Werkoff, Romain Bosc, et al. “Efficacy of Injecting Platelet Concentrate Combined with Hyaluronic Acid for the Treatment of Vulvovaginal Atrophy in Postmenopausal Women with History of Breast Cancer.” Menopause 25, no. 10 (2018): 1. https://doi.org/10.1097/GME.0000000000001122.
Krastev, Todor, Arjen van Turnhout, Eline Vriens, Luc Smits, and René van der Hulst. “Long-Term Follow-up of Autologous Fat Transfer vs Conventional Breast Reconstruction and Association With Cancer Relapse in Patients With Breast Cancer.” JAMA Surgery, October 10, 2018. https://doi.org/10.1001/jamasurg.2018.3744.
Kronowitz, Steven J., Cosman Camilo Mandujano, Jun Liu, Henry M. Kuerer, Benjamin Smith, Patrick Garvey, Reshma Jagsi, Limin Hsu, Summer Hanson, and Vicente Valero. “Lipofilling of the Breast Does Not Increase the Risk of Recurrence of Breast Cancer: A Matched Controlled Study.” Plastic and Reconstructive Surgery 137, no. 2 (February 2016): 385–93. https://doi.org/10.1097/01.prs.0000475741.32563.50.
Petit, Jean Yves, Patrick Maisonneuve, Nicole Rotmensz, Francesco Bertolini, Krishna Bentley Clough, Isabelle Sarfati, Katherine Louise Gale, et al. “Safety of Lipofilling in Patients with Breast Cancer.” Clinics in Plastic Surgery 42, no. 3 (July 2015): 339–44. https://doi.org/10.1016/j.cps.2015.03.004.
Platt, Dieter, ed. Geriatrics 2. Berlin, Heidelberg: Springer Berlin Heidelberg, 1983. https://doi.org/10.1007/978-3-642-68217-9.
Sakai, Shigeki, Naohiro Ishii, Yukie Nakamura, Kyoichi Matsuzaki, Shigemi Sakai, and Kazuo Kishi. “Complications and Surgical Treatment of Breast Augmentation Using Autologous Fat Transfer and Fillers.” Plastic and Reconstructive Surgery Global Open 9, no. 8 (August 16, 2021): e3734. https://doi.org/10.1097/GOX.0000000000003734.
Urbaniak, Camilla, Gregory B. Gloor, Muriel Brackstone, Leslie Scott, Mark Tangney, and Gregor Reid. “The Microbiota of Breast Tissue and Its Association with Breast Cancer.” Edited by H. Goodrich-Blair. Applied and Environmental Microbiology 82, no. 16 (August 15, 2016): 5039–48. https://doi.org/10.1128/AEM.01235-16.
“Vampire Breast Lift (R) | Official Website | Reviews | Find Provider.” Accessed November 28, 2024. https://vampirebreastlift.com/.
Visconti, Giuseppe, and Marzia Salgarello. “Magnetic Resonance Imaging and Ultrasound Evaluation after Breast Autologous Fat Grafting Combined with Platelet-Rich Plasma.” Plastic and Reconstructive Surgery 133, no. 4 (April 2014): 593e–94. https://doi.org/10.1097/PRS.0000000000000029.
Vizcay, Macarena, Shivangi Saha, Arbab Mohammad, Lee L.Q. Pu, Kotaro Yoshimura, Guy Magalon, Roger Khouri, Sydney Coleman, Gino Rigotti, and Stefania DeFazio. “Current Fat Grafting Practices and Preferences: A Survey from Members of ISPRES.” Plastic and Reconstructive Surgery – Global Open 11, no. 3 (March 2023): e4849. https://doi.org/10.1097/GOX.0000000000004849.
Tags
fat transfer, breast augmentation, Vampire Breast Lift®, PRP, platelet-rich plasma, breast cancer, recurrence rates, re-biopsy, mastectomy, microbiome, antibacterial, growth factors, breast reconstruction, in vitro studies, mice studies, apoptosis, breast cancer prevention, menopausal dryness, dyspareunia, anterior vaginal wall, breast cancer recurrence, PRP safety, breast enhancing lollipop, Vampire Breast Lift® consent, PRP prophylaxis, clinical trials, growth hormone, plastic surgery, PRP and scarring, scar treatment, port scars, breast health, regenerative medicine, PRP research, Charles Runels
Helpful Links
=> Next Hands-On Workshops with Live Models <=
=> Dr. Runels Botulinum Blastoff Course <=
=> The Cellular Medicine Association (who we are) <=
=> Apply for Online Training for Multiple PRP Procedures <=
=> FSFI Online Administrator and Calculator <=
=> 5-Notes Expert System for Doctors <=
=> Help with Logging into Membership Websites <=
=> The software I use to send emails: ONTRAPORT (free trial) <=
=> Sell O-Shot® products: You make 10% with links you place; shipped by the manufacturer), this explains and here’s where to apply <=
|
1-888-920-5311 |
[1] “Vampire Breast Lift (R) | Official Website | Reviews | Find Provider.”
[2] Kronowitz et al., “Lipofilling of the Breast Does Not Increase the Risk of Recurrence of Breast Cancer.”
[3] Visconti and Salgarello, “Magnetic Resonance Imaging and Ultrasound Evaluation after Breast Autologous Fat Grafting Combined with Platelet-Rich Plasma.”
[4] Vizcay et al., “Current Fat Grafting Practices and Preferences.”
[5] Kronowitz et al., “Lipofilling of the Breast Does Not Increase the Risk of Recurrence of Breast Cancer.”
[6] Krastev et al., “Long-Term Follow-up of Autologous Fat Transfer vs Conventional Breast Reconstruction and Association With Cancer Relapse in Patients With Breast Cancer.”
[7] Petit et al., “Safety of Lipofilling in Patients with Breast Cancer.”
[8] Sakai et al., “Complications and Surgical Treatment of Breast Augmentation Using Autologous Fat Transfer and Fillers.”
[9] Eichler et al., “Platelet-Rich Plasma (PRP) in Breast Cancer Patients.”
[10] Eichler et al., “Platelet-Rich Plasma (PRP) in Oncological Patients.”
[11] Urbaniak et al., “The Microbiota of Breast Tissue and Its Association with Breast Cancer.”
[12] Platt, Geriatrics 2.
[13] Asghar et al., “Efficacy and Safety of Intralesional Normal Saline in Atrophic Acne Scars.”
[14] El-Amawy and Sarsik, “Saline in Dermatology.”
[15] Hersant et al., “Efficacy of Injecting Platelet Concentrate Combined with Hyaluronic Acid for the Treatment of Vulvovaginal Atrophy in Postmenopausal Women with History of Breast Cancer.”

It’s great to see ongoing research and discussion around the effectiveness of PRP and the P-Shot® for men’s sexual health,…