|
Journal Club with Pearls & Marketing 2024.10.29 Cellular Medicine Association |
JCPM2024.10.29
The following is an edited transcript of the Journal Club with Pearls & Marketing (JCPM) of October 29, 2024, with Charles Runels, MD.
>-> The pdf of the transcript of this live journal club can be seen here <-<
Topics Covered
- Can You Do a P-Shot® and a GAINSWave Treatment on the Same Day?
- Multiple Sclerosis (MS) and the Ignored Research
- MS, Urinary Incontinence, and the O-Shot® Procedure

Charles Runels, MD
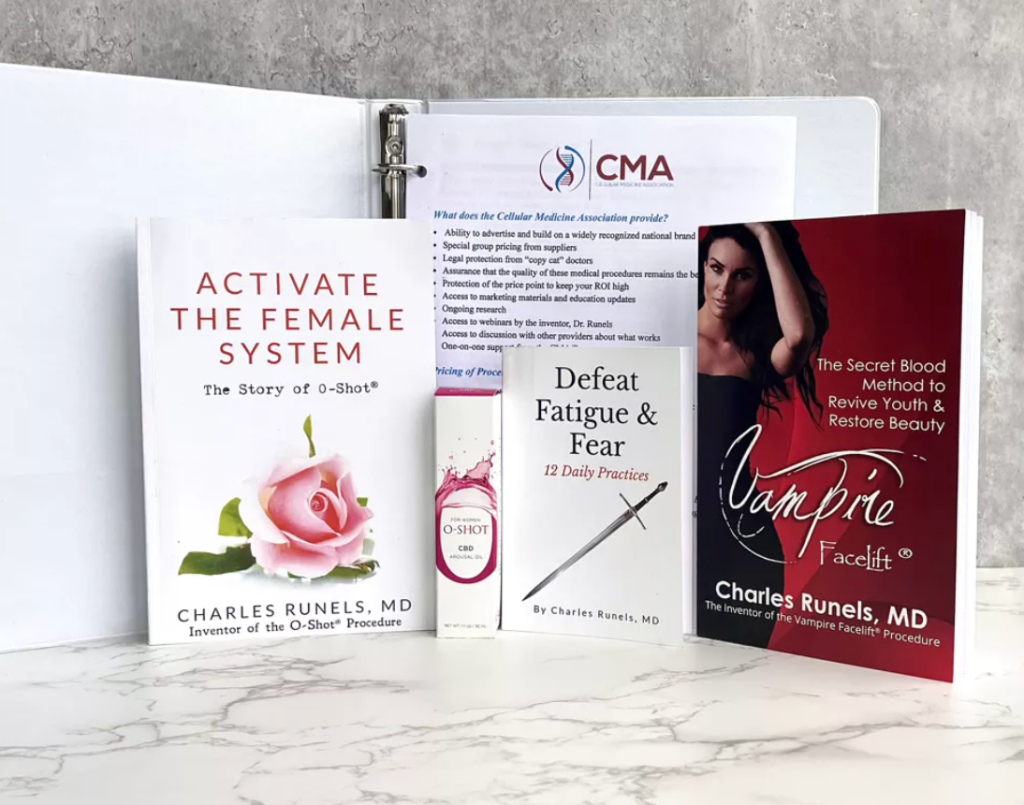
Author, researcher, and inventor of the Vampire Facelift®, Orchid Shot® (O-Shot®), Priapus Shot® (P-Shot®), Priapus Toxin®, Vampire Breast Lift®, and Vampire Wing Lift®, & Clitoxin® procedures.
Transcript
Charles Runels, MD:
Thank you for being on the webinar tonight.
I had a couple of questions come up in the past few days that I think are worth talking about.
The first one I’ve answered a few times. A new provider who wants to know, can I do a GAINSWave? It’s the second question about MS that I think I want to rant about: the research that’s been around for 20 years that maybe isn’t thought about as much as it should be.
Can You Do a P-Shot® Procedure and a GAINSWave Treatment on the Same Day?
But we’ll start with the easy one: “I’ve got a GAINSWave machine, and I know the protocol. I’m also doing the P-Shot® procedure. Can you do them both on the same day? And if so, which do you do first?”
You can do both (shock wave and P-Shot®) on the same day, and there is some synergy.[1] [2] [3] [4]
No one has done the study to see in which order of the the two procedures should be done. This is my reasoning, and again, I stand to be corrected, but my reasoning is that we know that of the chemotactic factors, the cytokines, the growth factors that are carried by platelets, many of them are small peptide chains: IGF-1, all these, VEG, they’re small peptide chains. And, of course, the power of the peptide is the code that it transcribes. Peptides are all the rage now, it seems when you’re talking about the new ideas in regenerative medicine.
But growth hormone’s a peptide, insulin’s a peptide. The reason there’s not an oral dosage for insulin is if you take it by mouth, you digest it, and the amino acids become no different than the Burger King you had. They’re just amino acids. They’re letters that have been de-scrambled.
So, when I see, for example, I don’t get it as much as I used to, but people say, “What about this oral growth hormone?”
Well, they’re saying it’s really oral growth hormone. You don’t believe it until you can take insulin by mouth because now it might be something that promotes growth hormone secretion, like arginine or glutamine, which, when taken on an empty stomach, can trigger the pituitary gland to release growth hormone.
But peptides are also important. Many of the powerful pituitary hormones and growth factors released from platelets are peptides.
So, let me return to our question: Can you use a GAINSWave on the same day? If so, in which order do you use it?
Again, no one’s done the research. I’ve done two studies looking at the effects of growth hormone when used for replacement in adults. One looked at pulmonary function, and the other looked at changes in VO2 max. One was with Saizen, and the other was with GENOTROPIN before it was sold by a pharmacy out of Pfizer.
When you mix growth hormone, you are not supposed to agitate it. You gently swirl it because it’s known that if you physically shake it, like you’re shaking up the protein powder in your breakfast drink, that you denature the proteins. Just the mechanics of shaking the bottle, the vial denatures growth hormone.
So my imagining is that if I inject platelets that are then activated and release small peptide chains, I may get a result. But it seems to me that if I’m hitting those peptides with a strong shockwave, I might be denaturing some of what I just went to a lot of trouble to put into the penis.
=>Next Hands-On Workshops with Live Models<=
Now, having said that, I know that some of our prominent providers will do the opposite. They’ll do PRP and then the GAINSWave, and they seem to get great results. We haven’t done the study. I don’t know if it makes a difference. But that’s the reasoning behind my recommendation: If you do the GAINSWave first and then the activated platelet-rich plasma, you will not risk denaturing the proteins for the small peptide chains with your shockwave.
That is not exactly the same, but it’s similar to the idea of the multiple papers that show if you laser the face and then apply platelet-rich plasma, you have more rapid healing after a facial laser and a better result than if you don’t use the PRP.
But imagine if you applied PRP and laser. Again, it’s not exactly the same idea, but the idea that if you apply energy from some source followed by PRP, you might get a better result. It seems logical, and there is nothing to lose and much to gain, I think, by doing it in that order.
Now, can you do it on the same day?
Absolutely, yes. I think you should be encouraged to do it on the same day because you’ve made something happen with your energy, whether it’s your shockwave or one of the radiofrequency devices. Either way, the PRP seems to be better applied afterward.
Multiple Sclerosis (MS) and the Ignored Research
Now, I’m going to rant a little bit about MS and then show you some research. I see Dr. George Ibrahim on the call, and I know that he has a special interest in this disease. And I have a special hatred for it and history with it treating it where I got beat up a little bit for using some of my ideas. So, I want to rant a little bit, and then I want to unmute Dr. Ibrahim. You guys are in for a real treat because Dr. Ibrahim enjoys a worldwide reputation. He’s truly brilliant. And one of the urologists in our group, whom I find inspiring and instructional.
The question from one of our members was as follows: “If you did an O-Shot on a woman with MS who’s using a catheter for urinary retention, would it help or hurt? What’s the recommendation?”
So, let me give you a little story about what’s happened with my practice up until this point. You know that I went broke twice. And the first time it was whatever, cliche, it happens, it was a divorce thing. The second time, I was told by the board to quit doing what I was doing with hormones because it was not in line with the American Board of Endocrinology. I didn’t lose my license, but they just said quit doing what you’re doing now. Now, all this happened 20 years ago; a lot has changed in the past 20 years.
In 1999, I heard someone lecture about using testosterone in women to help with migraines. And I plowed in the research, and at that time, we were talking 24 years ago, so I’m giving you a timeframe; this is what I want you to focus on. We’ll get back to the MS. I’m just talking about testosterone in men and women. In 1999, mostly bodybuilders were using testosterone. We weren’t replacing men very much. The A4M meeting was very small. But I heard a man lecture about using it to help prevent migraines in women who had menstrual-associated migraines. And I started reading.
A lady, Susan Davis[5], out of Australia, I discovered, had published multiple papers about the ability of testosterone to attenuate autoimmune diseases in females, including MS and lupus. And it was the evidence … Now this would’ve been, here’s the timeframe, ’64, and when you just search testosterone in MS and you search it by date, and so most recent, and there’s a lot that’s most recent, so there’s stuff out that came out this month that I’ll come back to. But if you do it in reverse order, then the first time it was sort of mentioned was in 1964, when I was four years old.
But then not much really happens until … Let me to do it the other way. Yeah. So this is 1964. And then you see almost nothing. And then you start to see it 20 years later in the eighties. This starts to be something that people were talking about.
Well, the only thing I know of in the autoimmune category that men get more than women is Reiter’s, which I never made that diagnosis. But anyway, except for that one-off, everything else, whether it’s rheumatoid arthritis, lupus, MS, it’s all more common in women. So, it makes sense—maybe, since men have more testosterone and women suffer more autoimmune diseases, maybe testosterone may be somewhat protective.
Susan Davis wrote a lot about this[6]. I performed hormone replacement for over 3,000 women in just a few years of opening my practice because this was before Suzanne Somers wrote her first books. And I was one of the only people really doing it—well, at least in the US.
But Europe and Japan, and especially Italy and Australia, I think, were ahead of us. And they didn’t have the burden of looking over their shoulder, which eventually tagged me for a while.
Of course, I now have an unrestricted license, but I got tagged for doing what I’m talking about here.
And it was no bad outcome, but it was, “Oh, you did this with this woman, and her testosterone level was higher than we thought it ought to be. This isn’t in line with the American Board of Endocrinology, so you have to quit doing hormones in the way you’re doing.”
So, that’s when I went broke the second time.
But back to this. You see, it doesn’t start coming up until the eighties. And if you look at the incidence of MS in men, it appears around the time of andropause, or at least more frequently. Multiple papers talk about it; testosterone levels and MS activity seem to correlate.[7] [8] [9] [10] [11] [12]
Now look, it’s more than 20 years, it was the eighties. We’re pushing 40 years ago. And this is what’s so maddening. When you look at the conclusion, “Further research is needed to better …”
Well, yeah, we need more research, but when do we get to start saying if you have MS, maybe someone should check your testosterone level and correct it, not to cure you, but possibly to attenuate the progression of the disease and perhaps at least for now make things better?
I did it repeatedly in my practice and almost lost my license because of it—not just for this indication but also for these and other indications.
Now, I need to unmute Dr. Ibrahim and let him catch up with us. Then we’ll get to the real question, which was, well, should you do an O-Shot if a woman has MS and urinary retention?
Hey George, can you hear me?
Can you hear me?
Charles Runels, MD:
I can, perfectly. Thank you for making time. I don’t think we ever talked about this, so I can’t wait to hear what you have to say. But I think you can see that I have a 20-year history of this soapbox of testosterone replacement to slow the progression of MS.
George Ibrahim, MD:
Well, first off, thank you so very much. And to the audience, Dr. Runels has been a wealth of information helping me in everything that I’ve done in my practice, and I cannot thank him enough.
I’ve been taking notes; earlier, you were talking about GAINSWave and when to do that in relation to doing the Priapus Shot. My practice always does. Anybody who signs up for a Priapus Shot comes in, and the first thing that after I’ve numbed them up, they will get GAINSWave to basically produce an iatrogenic injury so that when I take the PRP, the platelets know where to go.
Charles Runels, MD:
Beautiful.
George Ibrahim, MD:
I mean, that’s boom, done. Everybody gets a GAINSWave before every P-Shot. The other thing is the pump that most practitioners use; they use your method. If I’m able to, I like to teach the patients how to use the pump before they undergo the procedure. Because, let’s be honest, the next day, things are a little bit uncomfortable, and the pump can be a little bit more cumbersome. So I want them to be comfortable prior to the procedure using the pump.
All right. Now I’m going to the MS. Please stop me because this is your show.
Charles Runels, MD:
No, no, no. Go for it. Yeah, go for it.
George Ibrahim, MD:
All right. So, for the audience, I was a practicing urologist, and I had to stop because of MS.
Then, I became more of an age management practitioner doing hormones, aesthetics, and rehabilitation medicine, which obviously includes the PRP, O-Shot, and P-Shot type procedures.
The O-Shot is a game changer for women with stress incontinence. Literally, if it had been available when I was practicing urology, I would’ve performed two-thirds fewer procedures for incontinence in women. It’s that good.
Urgency, that’s more of an MS issue.
=>Next Hands-On Workshops with Live Models<=
So, when I started doing it, I thought, okay, I don’t know, my thoughts were to patients, I’ve said, “This is not going to hurt you, it may help.”
Well, damn, I kept seeing it help. And urge incontinence is not something you really would think about as what PRP does when we’re doing it for stress. But damned if it didn’t help.
Urinary retention, it helped that too.
I have no idea, Charles, the science—and I’m a urologist—on how it helped on the retention side. Maybe it was helping out with inflammation near the detrusor muscle. But I’ve seen it help those who have it the other way around. So that’s the thing about women.
For me personally, when I was in my early forties, one and done, that was it. And then, I got introduced to Dr. Runels’ method with a Priapus Shot®. And once I started doing that, I became pretty reliable, more than once on a given night. And that was huge because that was one of the biggest setbacks that MS had on my side; the male side was on the sexual aspect of it.
For me, I do mine every six months. My daughter practices with me; she’s going to be hearing this, so I don’t want to say much more.
Charles Runels, MD:
We get the point. It’s good.
George Ibrahim, MD:
But she’s heard this. And then, on the hormone side, damned if once I started to learn about stuff like this, I got mine checked; my levels were way lower than you would expect for somebody my age at that time.
Now, would I ever get on a platform at an MS Society meeting and tell patients this is the be-all and end-all? I have reservations about that. I can only share my personal experience, which has been fantastic. And now I’ll stop talking.
Charles Runels, MD:
Well, I have questions. I agree first with everything you said. And I should reemphasize, I say it occasionally, but I think your idea about giving, back up some, giving out the pump before people actually come for the P-Shot, if you can arrange that, is brilliant. Because many of the nuisance side effects that people may blame on the P-Shot are actually just from overusing or not understanding the use of the pump.
But back to MS. I have treated not hundreds, but I’ve probably treated 50 people who had MS that came to me. And just by correcting their testosterone level, they were better. Again, I would never say it was the cure.
But part of what I wanted to show with that screenshot was that there really is an impressive stack of papers showing that testosterone levels could be correlated with MS activity, and there may be some protection from MS by replacing testosterone.
So if you were talking to a physician, had this woman come in, because they sent me that question this week, who has urinary retention, she’s got MS. Would you include as part of the treatment protocol checking testosterone levels with the idea that at the worst it might slow the progression if we corrected lower levels? Or is it even that a stretch?
George Ibrahim, MD:
No, I would do it in a heartbeat. First of all, it’s like you’re not cutting off somebody’s stuff, so try it. I mean, you’re not going to hurt them. And it’s amazing. Sometimes, you’ll hear people call you back in a week or two and go, OMG.
Charles Runels, MD:
Yeah, exactly.
George Ibrahim, MD:
But it’s not going to hurt them.
Charles Runels, MD:
Right. Worst case scenario, they get a little acne and ask you to stop it.
George Ibrahim, MD:
Yeah, it gives them oily skin.
Charles Runels, MD:
So can I give you my theory about why I think the O-Shot might be helping?
George Ibrahim, MD:
Yeah.
Charles Runels, MD:
Because we’ve talked before about the amount of research that needs to be done, I think it’s going to take probably two more lifetimes to flesh out what’s possible and what’s not possible.
First, we know PRP has some neurogenesis properties,[13] but of course, MS is more central. But let me put it to you differently. Okay, not apples to apples.
But if someone has emphysema, and you put them through pulmonary rehab, you don’t make their lungs better. You are not  improving their lungs. They still have a reversible lung disease. But you can truly improve their VO2 max by increasing the number of mitochondria (by training the muscles), by strengthening the diaphragm, and even by some weight loss. And so, they’re able to burn more milliliters of oxygen per kilogram of body weight.
improving their lungs. They still have a reversible lung disease. But you can truly improve their VO2 max by increasing the number of mitochondria (by training the muscles), by strengthening the diaphragm, and even by some weight loss. And so, they’re able to burn more milliliters of oxygen per kilogram of body weight.
You have not really made their lungs better. But you made their life better.
And so my thinking is that, again, it’s not apples to apples, but even if we’re not reversing the MS with an O-Shot, if there’s just muscle atrophy, if there’s some un-coordination because there’s some, as we know with aging, DeLancey did all that work and others, with aging, there’s a decreased number of both muscle fibers and nerve fibers in the urinary sphincter. And if we’re helping improve what’s there, even if central function isn’t optimal, then what’s there might function better just because of that.
So that’s my theory. I don’t know how you even test it. It may be just about as real as the Easter Bunny. But that’s because I’ve observed the same thing with testosterone and with the O-Shot: people get better. But I don’t have a good explanation; I just have a guess.
George Ibrahim, MD:
When I give talks, probably one of my first slides is a pyramid, and the base of the pyramid, of course, the foundation stones are the biggest, and across the bottom, it says hormone optimization. And then everything else above, the top, is things like the P-Shot, O-Shot, and other things. But the whole point of that was when we were the healthiest, our hormones were basically the best optimized ever. Optimizing hormone. My thought is we used to think that our hormones went down as we got older. I think that we get older because our hormones go down.
Charles Runels, MD:
Definitely a negative feedback loop; they have to influence each other.
George Ibrahim, MD:
Yeah. And so many autoimmune diseases get better when the hormones are optimized.
Charles Runels, MD:
My basic training was an internist, and that’s such an old-fashioned name, I think it’s almost like, I don’t know, it’s almost like going on a house call with an old-fashioned stethoscope in a carriage, I don’t know if people even talk about internal medicine much anymore. But it meant you’re supposed to be able to diagnose people. The hard diagnosis, you’re supposed to figure it out. I trained in Birmingham, where Tinsley Harrison was the guy; that’s where he was. And I thought I was decent at it. I wasn’t the best, but I thought I was pretty good at it.
But sometimes I’d have people come to me, actually after I went all cash, I was better at it because I had more time to think about people and solve some hard cases, but one of the things that I did was someone who already been to three tertiary centers and nobody’s made them better yet, is just what you’re talking about. Is there this innate programming in our mechanism, our body, that wants to be well?
If you don’t know what else to do, make the body as healthy as you can, and it’ll figure it out a lot of the time and get well. You don’t even know what you did, but it just got better. And that starts with good hormone replacement.
George Ibrahim, MD:
Yeah. Well, first of all, please don’t downplay yourself. As a surgeon, we look at the internists as the ones with the brains. We would cut things out and throw things away.
But when it comes to hormone replacement, if you’re not hurting somebody, try it.
Charles Runels, MD:
Okay. So, let’s return to this question. I’m so glad you jumped on the call. I know it was last minute, so thank you for jumping on the call. So, if you were talking to this woman who has a patient with urinary retention and is wondering if an O-shot might make it better or worse, what would you say to them?
George Ibrahim, MD:
I’d say, “Ms. Jones, the only thing this is going to be is going to be a stick. The worst side effect is going to be a bruise. This is your own body’s materials being replaced in a fashion that tends to heal things. It may or may not work. What’s the risk? All it is going to be the cost of this visit. Let’s see.”
Charles Runels, MD:
She’s already using a catheter, so just keep using your catheter?
George Ibrahim, MD:
Yeah. And I’d go, “And I don’t have a crystal ball, I just know that I’ve done this many, many times, and the majority of the people that I’ve done this on with your issue have seen positive results.”
And that’s how I pose it.
Charles Runels, MD:
What do you think about it? We haven’t talked about this yet either; it’s been a while since we caught up; what do you think about using the botulinum toxin for erectile function and/or urinary or sexual function in women who might have MS, does it change anything?
George Ibrahim, MD:
Okay, now that’s a great question because I do use neuromodulators in both men and women. But I’ve not used it as a specific treatment for MS. That’s a great question to ask.
I know it has a sexual way of enhancing things, it’s been crazy. But I mean, for females, I mean, crazy for men, it has helped with erectile dysfunction. For women, you’re the one that’s got the best description of that, like the lizard brain. But as far with MS, as a urologist, we would do it in the detrusor muscle through the cystoscope, we would do it through the bladder. I have not done toxins for MS patients, no, I’ve not done that yet.
Charles Runels, MD:
Can I give you a guess? And you just tell me, give me feedback.
George Ibrahim, MD:
Yeah, sure.
Charles Runels, MD:
I want people to tell me when I sound like I’m off track. But okay. So, here’s what my sweet bride has noticed, because she’s a gynecologist and has treated a lot of incontinence as well. And she did the stats on the paper we published about using botulinum toxin in women. Anecdotally, she has treated quite a number of women with severe urge incontinence by injecting the clitoris. And her idea is that, and with great success, her idea is that it somehow might be acting centrally in the same way that it acts when we treat sexual dysfunction.
And the part of her reasoning behind that is if you actually look at the amount of Botox that’s being used, it doesn’t match up with how much we use in the face. In other words, there it’s wide open, it’s all anecdotal, it’s all speculation. But we have some anecdotal cases of severe urge incontinence getting better. Just injecting the clitoris somehow may be triggering something in the ganglion. So, I don’t know. Go ahead.
George Ibrahim, MD:
Well, let me tell you where I would go with this. I’ve made sure that my medical assistants have things set up so that I’m not injecting the toxin when I’m doing the G-spot injection, when I’m doing the typical O-Shot injections.
But that G-spot is right under the detrusor.
Charles Runels, MD:
Interesting.
George Ibrahim, MD:
If you’ve got a woman in retention, why not do it?
Charles Runels, MD:
Yeah, interesting.
George Ibrahim, MD:
Because that’s on the other side of where I would inject, and I was coming through with a cystoscope.
Charles Runels, MD:
Yes, I’d love to see it; that’s the kind of stuff I would never know. I’m in Salt Lake to do a lecture here at the AMMG meeting. And this is my second honeymoon, not a second honeymoon, our second anniversary, and my wife is sitting here fidgeting. I know she wants to say something. Have you met George yet? You’re going to-
Alexandra Runnels, MD:
Not in person.
Charles Runels, MD:
No. You’re going to love him when you meet him. I know you’re fidgeting, talk to him, surgeon to surgeon, because you want to say something, I can tell. She’s sitting there listening to me. So talk about whatever you need to say because I know that you have something.
Alexandra Runnels, MD:
Hey there, George.
George Ibrahim, MD:
Hello.
Alexandra Runnels, MD:
Nice to talk with you.
George Ibrahim, MD:
Nice to meet you virtually.
Well, I loved hearing what all you had to say so far tonight. And I know you’ve got a wealth of knowledge and wealth of experience under your belt.
But Charles is right; I was fidgeting because one of the most exciting things that has happened for me in my career really was the discovery that when we were doing the study looking at putting botulinum toxin (BoNT) into the clitorises of the female patients for sexual function, the patients were spontaneously telling me, without being prompted, coming in and saying, “My sex is great, but what’s crazy is my urge incontinence is gone.”
And all I did was put the BoNT into the clitoris, nowhere else.
George Ibrahim, MD:
Wow.
Alexandra Runnels, MD:
And I heard it more than once. And then I experienced it personally, my own self, my own urge incontinence resolved with just BoNT in the clitoris.
Charles Runels, MD:
You think he got his idea of putting a dot right here up in the anterior vaginal wall.
Alexandra Runnels, MD:
Yes, I like it. And there’s also; there’s a paper I read not that long ago, but within the last year or two, of an urogynecologist that was looking at doing a trans vaginal singular injection into the bladder, into the trigone of the bladder, I believe, of botulinum toxin rather than going with the cystoscope. So I think it’s a similar idea.
I mean the nerve, the innervation of the urethra, the clitoris, the bladder, it’s all sorts of complex tangled up web anyway that it’s hard to imagine. So it’s hard to imagine that you’re not affecting one structure when you’re treating the other; they’re all connected. I mean, they’re all connected.
And it’s always never made sense to me either is with, and I did it for, as a gynecologist, many times with the cystoscope in the bladder, when you inject BoNT into the detrusor muscle through the cystoscope, I’ve never been able to wrap my head around the fact that, okay, well, when you use it in the face for wrinkles, you’re paralyzing skeletal muscle. And it doesn’t take that many units in facial muscles to cause complete paralysis. But often, there’s a big difference between how much paralysis you get by adjusting the number of units very little. Okay.
So it’s never made a whole lot of sense to me that the mechanism of action in the bladder for helping with incontinence and decreasing overactive detrusor muscle behavior is so easily treated with just a standard number of units spread out throughout the bladder. But you still have bladder function, it doesn’t paralyze it, it just supposedly attenuates it. But doesn’t make sense when you think about it with working the same way as it does in the face.
So I think what’s happening is the clitoris, with all of its many, many, many nerve endings that is acting as a port to the pelvic ganglion where the actual neuromodulation is occurring that is affecting all of the organs in the pelvis, in the genitalia, the bladder, in the urethra and the clitoris, I think that’s where the neuromodulation event is occurring. And I don’t think that urologists need to be doing it through the cystoscope anymore is what I have to one day foresee possibly being something that happens.
And it makes sense to me. And I don’t know, you correct me. But all of the other versions of neuromodulation for bladder dysfunction, like in neurogenic bladders and spinal cord injury patients and urge incontinence, so whether we’re talking about sacral neuromodulation or percutaneous tibial neuromodulation, all of those varieties of neuromodulation are … it’s just Botox is another version of neuromodulator. It’s just a chemical neuromodulator versus the electrical stimulation or whatever.
There’s so much to be done in this field, and it’s just super exciting to me. I’ve been dying for Charles to let me talk about it out loud and to hear what other people have to say about it.
George Ibrahim, MD:
And I try to screen my prospective patients as to whether it’s stress or urge. But I’ll have patients that have been patients, and we start talking about incontinence, and long story short is their story relates it to be urge and next thing you know, I’m doing the O-Shot, but I’m putting toxin in. And damned if they’re not … it helps. And so, I mean, it works.
Again, when I say it works, I’m going to say it works in enough people that I can say that out loud. I won’t put it in print because I can never promise anybody anything. But it really has been a game changer. And it’s so much easier to get there.
Charles Runels, MD:
Easier for the patients of course.
George Ibrahim, MD:
Yeah. They don’t have to have-
Charles Runels, MD:
I don’t ever wake up in the morning and say I want to have a cystoscope after my coffee.
George Ibrahim, MD:
Yeah. Now, for females, it’s a lot easier, but it’s still not a fun thing.
Alexandra Runnels, MD:
And you avoid that post-scope Botox infection that happens in 15% of the patients.
Charles Runels, MD:
Yeah. Well, I’m so glad you jumped on the call tonight. I always learn from you, George. I know we’ve talked about getting together soon and planning some research. I’ve got some more funds available that I want to share with you. So, unless you have something else, I think we’ll call tonight. Thank you for giving me this virtual you.
George Ibrahim, MD:
Thank you for your time and for all your contributions to my education.
Charles Runels, MD:
All right. Thank you, George. Good night.
George Ibrahim, MD:
Good night.
=>Next Hands-On Workshops with Live Models<=
References
Asbelaoui, Narimène, Charly Abi-Ghanem, Géraldine Schlecht-Louf, Hania Oukil, Cindy Degerny, Netherlands Brain Bank, Michael Schumacher, and Abdel Mouman Ghoumari. “Interplay between Androgen and CXCR4 Chemokine Signaling in Myelin Repair.” Acta Neuropathologica Communications 12, no. 1 (January 30, 2024): 18. https://doi.org/10.1186/s40478-024-01730-1.
Davis, Susan R. “When to Suspect Androgen Deficiency Other than at Menopause.” Fertility and Sterility 77 (April 2002): 68–71. https://doi.org/10.1016/S0015-0282(02)02977-1.
Dougados, M., K. Nahoul, L. Benhamou, P. Jungers, D. Laplane, and B. Amor. “[Study of plasma androgens in women with autoimmune diseases].” Revue Du Rhumatisme Et Des Maladies Osteo-Articulaires 51, no. 3 (March 1984): 145–49.
Geng, Chaofan, and Yi Tang. “Association between Levels of Sex Hormones and Risk of Multiple Sclerosis: A Mendelian Randomization Study.” Acta Neurologica Belgica, July 29, 2024. https://doi.org/10.1007/s13760-024-02613-x.
Geyik, Serdar. “Comparison of the Efficacy of Low-Intensity Shock Wave Therapy and Its Combination with Platelet-Rich Plasma in Patients with Erectile Dysfunction.” Andrologia 53, no. 10 (2021): e14197. https://doi.org/10.1111/and.14197.
Hammad, Muhammed A. M., Adriana Rush, Charles A. Loeb, Jasmin Banton, Elia Abou Chawareb, Narmina Khanmammadova, Rafael R. Gevorkyan, David W. Barham, Faysal A. Yafi, and Lawrence C. Jenkins. “Multiple Sclerosis and Hypogonadism: Is There a Relationship?” Sexual Medicine Reviews 12, no. 2 (March 26, 2024): 178–82. https://doi.org/10.1093/sxmrev/qead050.
Narasimman, Manish, Max Sandler, Ari Bernstein, Justin Loloi, Russell G. Saltzman, Helen Bernie, and Ranjith Ramasamy. “A Primer on the Restorative Therapies for Erectile Dysfunction: A Narrative Review.” Sexual Medicine Reviews, March 17, 2024, qeae012. https://doi.org/10.1093/sxmrev/qeae012.
Sánchez, Mikel, Eduardo Anitua, Diego Delgado, Peio Sanchez, Roberto Prado, Gorka Orive, and Sabino Padilla. “Platelet-Rich Plasma, a Source of Autologous Growth Factors and Biomimetic Scaffold for Peripheral Nerve Regeneration.” Expert Opinion on Biological Therapy 17, no. 2 (February 1, 2017): 197–212. https://doi.org/10.1080/14712598.2017.1259409.
Shah, Jainik, Maximilian G. Fidel, Dhiraj S. Bal, Armin Kharazi, Connor F. Roque, Yool Ko, Karim Sidhom, David Bouhadana, Francis Petrella, and Premal Patel. “An Overview of the Canadian Landscape on the Use of Restorative Therapies for Erectile Dysfunction and Peyronie’s Disease.” Canadian Urological Association Journal 18, no. 12 (July 15, 2024). https://doi.org/10.5489/cuaj.8804.
Sicotte, Nancy L., Barbara S. Giesser, Vinita Tandon, Ricki Klutch, Barbara Steiner, Ann E. Drain, David W. Shattuck, et al. “Testosterone Treatment in Multiple Sclerosis: A Pilot Study.” Archives of Neurology 64, no. 5 (May 2007): 683–88. https://doi.org/10.1001/archneur.64.5.683.
Towe, Maxwell, Akhil Peta, Russell G. Saltzman, Navin Balaji, Kevin Chu, and Ranjith Ramasamy. “The Use of Combination Regenerative Therapies for Erectile Dysfunction: Rationale and Current Status.” International Journal of Impotence Research, July 12, 2021, 1–4. https://doi.org/10.1038/s41443-021-00456-1.
Wei, T., and S. L. Lightman. “The Neuroendocrine Axis in Patients with Multiple Sclerosis.” Brain: A Journal of Neurology 120 ( Pt 6) (June 1997): 1067–76. https://doi.org/10.1093/brain/120.6.1067.
Tags
Charles Runels MD, webinar, GAINSWave, P-Shot, O-Shot, platelet-rich plasma (PRP), peptide therapy, growth factors, regenerative medicine, shockwave therapy, cytokines, MS (multiple sclerosis), testosterone therapy, autoimmune disease, hormone replacement, sexual health, urinary retention, urge incontinence, stress incontinence, Botox, botulinum toxin, neuromodulation, neurogenic bladder, pelvic health, cystoscopy, clitoral injections, detrusor muscle, sacral neuromodulation, sexual dysfunction, regenerative urology, urogynecology, medical research, clinical practice, hormone optimization, medical education, George Ibrahim MD, Alexandra Runnels MD, inflammation, neurogenesis, regenerative procedures, webinar transcript
Helpful Links
=> Next Hands-On Workshops with Live Models <=
=> Dr. Runels Botulinum Blastoff Course <=
=> The Cellular Medicine Association (who we are) <=
=> Apply for Online Training for Multiple PRP Procedures <=
=> FSFI Online Administrator and Calculator <=
=> 5-Notes Expert System for Doctors <=
=> Help with Logging into Membership Websites <=
=> The software I use to send emails: ONTRAPORT (free trial) <=
=> Sell O-Shot® products: You make 10% with links you place; shipped by the manufacturer), this explains and here’s where to apply <=
|
Charles Runels, MD 888-920-5311 CellularMedicineAssociation.org |
Page of |
[1] Narasimman et al., “A Primer on the Restorative Therapies for Erectile Dysfunction.”
[2] Shah et al., “An Overview of the Canadian Landscape on the Use of Restorative Therapies for Erectile Dysfunction and Peyronie’s Disease.”
[3] Towe et al., “The Use of Combination Regenerative Therapies for Erectile Dysfunction.”
[4] Geyik, “Comparison of the Efficacy of Low-Intensity Shock Wave Therapy and Its Combination with Platelet-Rich Plasma in Patients with Erectile Dysfunction.”
[5] Davis, “When to Suspect Androgen Deficiency Other than at Menopause.”
[6] Davis.
[7] Geng and Tang, “Association between Levels of Sex Hormones and Risk of Multiple Sclerosis.”
[8] Asbelaoui et al., “Interplay between Androgen and CXCR4 Chemokine Signaling in Myelin Repair.”
[9] Hammad et al., “Multiple Sclerosis and Hypogonadism.”
[10] Dougados et al., “[Study of plasma androgens in women with autoimmune diseases].”
[11] Sicotte et al., “Testosterone Treatment in Multiple Sclerosis.”
[12] Wei and Lightman, “The Neuroendocrine Axis in Patients with Multiple Sclerosis.”
[13] Sánchez et al., “Platelet-Rich Plasma, a Source of Autologous Growth Factors and Biomimetic Scaffold for Peripheral Nerve Regeneration.”



It’s great to see ongoing research and discussion around the effectiveness of PRP and the P-Shot® for men’s sexual health,…