|
Journal Club with Pearls & Marketing 2024.10.08 Cellular Medicine Association |
JCPM2024.10.08
The following is an edited transcript of the Journal Club with Pearls & Marketing (JCPM) of October 8, 2024, with Charles Runels, MD.
>-> The pdf transcript of this journal club can be downloaded here <-<
Topics Covered
- The Injection of PRP into the corpus cavernosum to treat erectile dysfunction
- A Review of Some of the Potential Uses of PRP in Dermatology
- PRP vs. HA vs. HA + PRP for the Knee
- P-Shot® is now the standard of care in some countries
- Very Difficult Problems in Gynecology that Improved with PRP
-
- Anal Sphincter Injury
- Anal Stenosis after Fournier’s Gangrene
- Why giving money back when there is no benefit helps you get people well
- Do you adjust PRP processing based on the patient’s platelet count?
- Can you swap out the hyaluronic products when doing the Vampire Wing Lift® procedure?
- Can you use Bellafill with the Vampire Wing Lift® procedure?
- A Chronic, Non-Healing, Vaginal Wound
- Long-Standing Severe Virginal Stenosis and Shortening of the Vagina Post Hysterectomy
- Post-partum, Chronic Fecal Incontinence made better with PRP
- References
- More Help and Useful Links

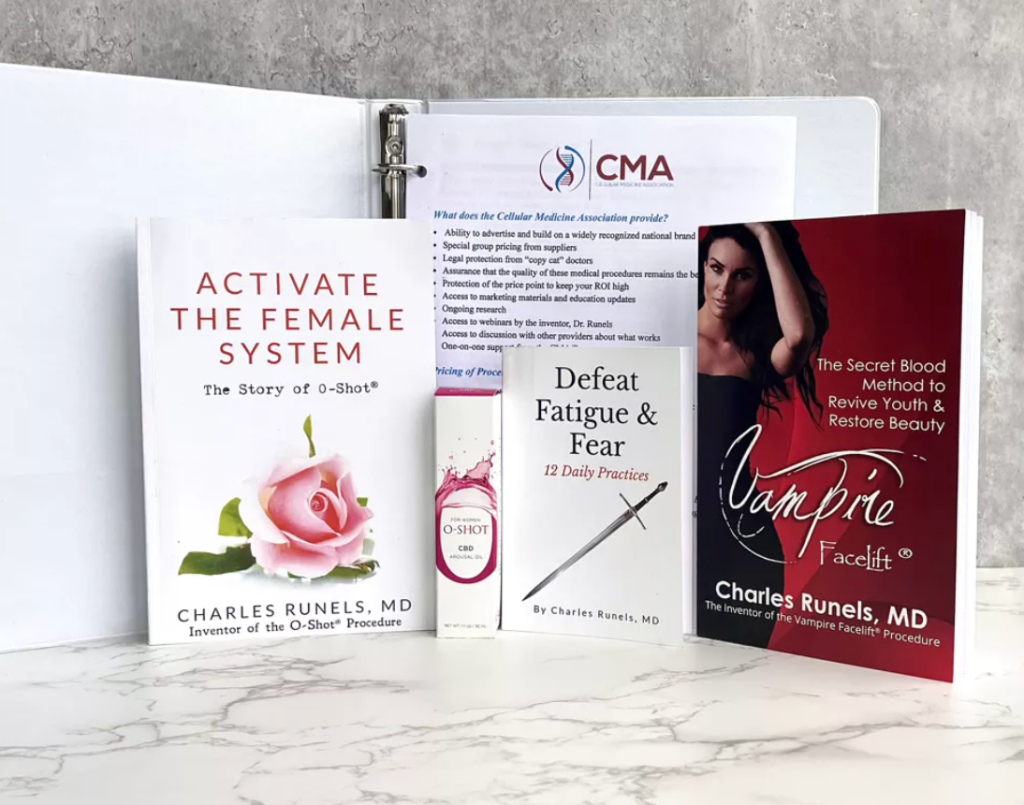
Charles Runels, MD
Author, researcher, and inventor of the Vampire Facelift®, Orchid Shot® (O-Shot®), Priapus Shot® (P-Shot®), Priapus Toxin®, Vampire Breast Lift®, and Vampire Wing Lift®, & Clitoxin® procedures.
Transcript
Charles Runels, MD:
Welcome to our Journal Club. Last week we had a special guest and lots of very instructive pictures, before and after, talking about using HA fillers to increase the girth of the penis. If you missed that, it’s been posted on the website. So, you should be able to find it, it would be the last one posted. They’re posted sequentially.
The Injection of PRP into the corpus cavernosum to treat erectile dysfunction
Let’s start with this one because they looked at using platelet-rich plasma for erectile dysfunction and showed no benefit.[1] So, let’s look at what they did and see if we should all quit doing P-Shots® or not.
I’ll give you the punchline, I think we’re still good to keep going.
Here’s the big thing that I found disturbing about their study, is that they chose people 20 to 80 years old. And if you look at the comorbidities, many of them had hypertension or diabetes, and they started the study by asking them to stop their ED therapy. I can’t find where they reported what percentage were taking PDE5 inhibitors, how much they were taking, or if there was a difference between those in the placebo arm and those not in the placebo arm.
With treatment, their SHIM scores stayed about the same. But if you stop my Viagra, and six months from now my erections are the same as they were on the Viagra, we might argue that that’s a benefit. Except, the placebo arm had the same change, which is also conflicting because, as you guys know, we have a stack of research showing that doing hydrodissection with saline is not a placebo.[2] [3] [4] [5] [6]
The other thing is that when they performed the procedure, they activated the platelets, but I can’t tell exactly what they did. It looks like maybe they were injecting PRF, although they call it PRFM.
Then, they did this long two-minute injection per corpus cavernosum and kept a tourniquet on for 20 minutes and a pressure bandage. Which, of course, a pressure bandage would be prone to compress the material out, was left on after the tourniquet came off. As you guys know, we don’t use a pressure bandage.
We use a vacuum device to pull more fluid, and more plasma, into the penis (not squeeze it out with a pressure bandage).
So I’m left wondering what this even means. But you need to know what’s out there that supports and what doesn’t support. And this one does not support, at least, the idea of injecting something that comes from plasma into the penis, although their protocol was significantly different from what we use.
Do not immediately stop PD5Is post-P-Shot® procedure
But this brings up a good point, which is, clinically, when I treat someone with the P-Shot® (if you don’t tell them specifically not to do so), they are prone to stopping everything, all their medications.
If you have someone that’s on Trimix, and they’re taking daily Cialis, and you give them a P-Shot®, and they’ll just stop both of those things and wonder why their erections got worse instead of better the next day—that’s why.
So, I explain it to patients as, “I want to do everything I can to improve your erections, and then we will back off things, one step at a time, and see what’s the minimal effective treatment.”
If you look at the scores of the men in this study, they started off with a score of around 15, on a scale of 25, so they were having erectile dysfunction while on their ED therapies.[7]
So, clinically speaking, I wouldn’t tell them, “Now stop your medicine, and let’s see how you look tomorrow after your P-Shot®.”
Normally, people cut their dose in half. So, they stay on their medication, and after somewhere between 6 and 12 weeks, they’ll be able to cut their Trimix dose in half. Or if they’re taking Viagra or Cialis, they’ll cut the dose in half. If they’re on a low dose, they might discontinue it completely.
But this is a very nebulous and very important thing that happened, which I think makes this study nearly impossible to interpret.
But I brought it out because it just came out, so you need to know about it. We’ll watch what happens in future studies and adjust accordingly.
This is the second time I’ve seen this long, prolonged injection. It looks like they did a retrograde injection through the corpus cavernosum over two minutes, trying to somehow prevent the platelets from being disrupted. But when you add calcium chloride, that’s exactly what you did: disrupt the platelets—that is why you added the CaCl.
So maybe there’s something about the basic science I’m missing. If there’s someone on the call who can call me out on it, please educate me. But I found this whole protocol to be mysteriously confusing. That brings me to the next one, which was a meta-analysis that showed the benefits of injecting the penis with PRP.[8]
I didn’t know there were these many studies. Surely that’s not 1,050 abstracts? But it can’t be 1.050. They went through what looked like 1,000 abstracts and came up with 13 studies that they found initially eligible.
And they narrowed it down to three double-blind prospective placebo-controlled studies.
Again, I don’t particularly prescribe the idea of saline as a placebo in a PRP soft tissue study, but I think we’re up to four that showed benefit and one that did not, this Masterson study. We’ve reviewed all of these already. But this meta-analysis was nice, and it showed benefits. Their conclusion was that when the evidence was pooled, the analysis revealed significantly greater attainment of improved erection in the PRP during the final follow-up, with significant improvements in their scores. 
So, they suggest longer-term follow-up and look at possibly combining the PRP with other regenerative medicines, or I would add modalities. I know that many of you are combining PRP with shockwave therapy. And, of course, we did the study with Judson-Brandeis, combining the P-Shot® procedure with nitrate enhancers and the pump, and demonstrated improved erection and growth of the penis.[9]
The pump alone, a vacuum device, has been shown to improve erections on its own.[10] [11] [12] [13]
So, this combination therapy of a vacuum device combined with shockwave therapy, plus PRP, is the perfect penis club.
It was encouraging to have this study[14] come out almost simultaneously with that one study that showed no benefit[15] (even though what they did was NOT a P-Shot® procedure protocol).
So those were the two studies that I wanted to show you about erection.
P-Shot® is now the standard of care in some countries
In this review article, metanalysis, I highlighted here that regenerative therapies have apparently become first-line therapy in some countries.
Here it is, the evidence regarding regenerative medicine. I call it cellular medicine, not because I don’t like the regenerative word, but because it just triggers some people. I am unsure why, but in some circles, that word, regenerative, somehow hints that it is not solid science. But whatever, that’s what they call it in this paper, and that would be the cellular therapies. And it’s growing, and even the EAU guideline is now recommended as part of the treatment for selected ED patients.[16]
So it’s going mainstream. There you go, those are the references. Which is, wow, that’s amazing. I did not know that it was going mainstream.
Anyway, so there you go. That was a very encouraging paper to see.
A Review of Some of the Potential Uses of PRP in Dermatology
This is a great one to share with your patients because it discusses a variety of things you can treat with PRP, all of which we’ve discussed.
It’s a nice review article; if you send it to your patients, almost everybody will have something on this list. We all have hyperpigmented or hypopigmented scars somewhere. Most people have some trauma scars, which we covered two weeks ago in our Journal Club[17], about PRP being helpful for that. And, of course, we’re always talking about helping with the aging face.
Unless you’re doing wound care, that part is probably not as interesting to you, but I think it has spillover effects on the other things we do. It testifies that even in a wound with poor circulation, you can have benefits.[18]
PRP vs. HA vs. HA + PRP for the Knee
I have one where they looked at intraarticular injections using pure HA versus HA with PRP, and they all showed benefits.[19]
We’ve talked about this a lot. In every study we’ve looked at, compared with corticosteroids, the pain is often relieved sooner with corticosteroids. But even as soon as three months out, you start to see more pain relief with PRP. In some studies, it’s enhanced when combined with HA. However, in this one, there was no difference. But both HA and PRP beat cortical steroids at six months, both in pain relief and in preservation of the joint, in multiple studies.
This one was not open source. I’m including a link to it, and I think that’s really all you need to get the gist of it. We’ve talked about it. It comes out so frequently now that I’m surprised it’s not standard of care.
Very Difficult Problems in Gynecology that Improved with PRP
The last paper is just a smorgasbord of chronic hard-to-treat problems, with case reports about what happened and what was done.[20]
Anal Sphincter Injury
Here’s an anal sphincter injury. I think it said this woman suffered for ten years or something like… Yeah, she went for 6 out of 10 pain for ten years. With horrible pain with touching, clothing, and, of course, sexual intercourse.
One month after treatment with PRP, she’s having sex and has minimal pain.
So, I think that’s a beautiful story.
Anal Stenosis after Fournier’s Gangrene
And here’s one of the anal stenosis after Fournier’s gangrene. These are horrible. I know some of you treated Fournier’s. But when I ran a wound care center, we did hyperbaric treatments. Imagine someone with Fournier’s on a ventilator with IV antibiotics running into them, and they’re in a hyperbaric chamber at two atmospheres, three atmospheres. These people are so sick, as you know. And this poor lady had a problem with stenosis that was made better after a PRP.
If you’re doing the O-Shot® and you send this out to your people, you will have people call.
It won’t be a hundred people calling you, but this is open source, so you can send a link to it to your people. This is a very good example of what helps motivate and instruct doctors about marketing.
It pains my soul when I see doctors trying to lure people in by saying 20% off. Imagine Superman saying, “Please, come see me tomorrow. I’ll give you 20% off.” You can treat people for free if you want if they have no money, but you have no reason to try to bait them into your office when you can do things like this for them. Now I always tell people, “If this doesn’t make you well, to the point you’re delighted with it, I won’t keep your money.”
And I do sometimes treat people for free. But the point I’m getting at is if you understand that there are people in your community who are suffering this way, and they haven’t read this research, they can’t read your mind.
And I don’t mean to be sarcastic, but I’m trying to communicate that they don’t know what you know.
If you take the position that, “Oh, if there’s someone in my community that’s suffering with this, I should let them know that this possibility exists.”
So I’ll email my people and say, “Hey, if you or someone you love suffers from this, let them know that there’s a potential way to treat it with a variation on our O-Shot® procedure, and they should contact us.”
It’s that simple.
It’s not literature; it’s nothing other than a motivated doctor trying to inform people about what they can do if they need relief.
That’s it.
And so I think, wow, we did it in 17 minutes. Let me see if anyone has questions or comments, and then we’ll call it a day.
Do you adjust PRP processing based on the patient’s platelet count?
Eric asks, “Should we adjust a PRP preparation based on the patient’s platelet count?”
Answer: No one really knows.
When I was teaching in Europe, Serbia, and other places, they would do a platelet count at the bedside. And if you look at the orthopedic literature, they talk much about cell counts. And you can dive into this, as you know, because you’ve been with us and you’ve read a lot of this basic research, you can dive into it and get esoteric.
The platelets work better if you draw the blood immediately post-aerobic exercise or if you wash them with saline and then reconstitute them.[21] [22] [23] [24] [25]
The farther I go, the more confused I get as I dive into the literature.
But I reassure myself by thinking, if someone operated on this person, if they had a tonsillectomy or hysterectomy, or if they just scraped their knee and we had to heal, would they be able to?
And I think that that’s a way, as a clinician, you can reassure yourself, “Oh, yeah, they’re healthy enough to heal from surgery.”
Apply for Online Training for All PRP Procedures
Or not.
Here’s someone who’s malnourished, and they’re on high-dose corticosteroids, and they’re on chemotherapy. For example, one study looked at women with alopecia on chemotherapy for breast cancer, and they were not able to respond to PRP.[26] They did respond to those cold packs on the scalp, for some reason, but minimally. So, if you’re treating alopecia in someone on chemotherapy for breast cancer, you wait until they’re through with their chemotherapy and their nutrition status is back up. And then, if you want to accelerate hair growth, you can.
But that’s how I settle out the question I don’t know how to answer.
Can you swap out the hyaluronic products when doing the Vampire Wing Lift® procedure?
I think they are interchangeable. I would probably avoid Voluma because it’s more prone to nodularity. I use either Juvederm, Juvederm Ultra Plus or the new Jeuveau. So, I don’t think that you need Voluma, but you could use it.
The biggest thing you’ll see with any of them, for some reason, post-Vampire Wing Lift® procedure, your patient will be more prone to be able to palpate some nodules. They’re not seromas or even granulomas; they’re more palpable for some reason. Probably the same thing that’s going on in the cheeks, but they feel it, and it goes away. As far as I know, everyone who’s had it, it’s gone away within a month or two. I could be wrong, but I would anticipate that it may be more likely with Voluma. But I don’t know. If you try it, let us know.
Based on what you’re looking at, I see a lot of variety in how much filler is used. I tend to want to see what happens with a smaller volume since we know adipocytes multiply and enlarge, multiply in number, enlarge in size, based on studies that Sclafani did back in 2010, 2009, was injected into the back of the arm and biopsied,[27] and based on what we see with our Vampire Breast Lift®. Injecting the breast is the only thing I do where it’s often more volume at two months than the day I did it.
With the face, you might get some resolution and not as much volume, but with the breast, the fat cells go crazy. And there’s fat in the labia majora, as you know. So, I think it’s worth doing a more conservative treatment where they see volume and increased rubor, and you give the fat cells a chance to multiply and enlarge. And if they don’t lose weight, they should see something that’s even more voluminous than the day you did it if they’re patient enough to wait a couple of months.
But I can’t argue about adding extra volume with your fillers or PRP. And that’s often done as part of the art of what you’re doing. You look at it, and with experience, you know what to do. The good thing is that you can always add more. Or, with your hyaluronic acid fillers, you can dissolve it with hyaluronidase.
Can you use Bellafill with the Vampire Wing Lift® procedure?
I’m not a big fan of Bellafill, and I know that was addressed some… Thanks for your question, Pete. It was addressed last week when Dr. Song talked about his penile procedures. Years ago, I heard Dr. Obagi, who I consider the godfather of cosmetic dermatology, was doing it before most people were talking about it much. I’ve heard the man lecture twice. If you ever get the chance, you should listen to him. He’s brilliant, a pioneer, and very aggressive. I don’t know what he does now, but at one time, he did chemical pills under general anesthesia, deeper and more aggressive than I would ever be willing to do.
I’m making a point that he’s experienced; he’s not bashful or timid. And yet I heard him say, more than once, that he never uses permanent fillers because permanent good can also be permanent bad. And I’ve seen some horror stories. One of them was in one of our own providers, where she had to have some of the permanent fillers removed.
And so, I’m not saying no, but in my practice, I say no.
Just be careful with it.
Oh, wow. Okay, good. So my wife, who’s a board-certified gynecologist, is in another town right now and listening. She said she had a couple of anecdotes or additions to add to what we’re talking about. Let me see if I can get her microphone to work.
Thank you, Alex. Hold on a second. She’s done a lot of O-Shots® and was an experienced gynecologist before I met her, so I’m curious about what she says about what we’re looking at. Let’s see. Your microphone should work now. If you want to turn it on, Alex.
Can you hear me okay?
Charles Runels, MD:
Yep, go for it.
Alexandra Runnels, MD, FACOG:
Well, thank you for everything that you talked about. This last article definitely got my attention: the article with the case series of these reports.[28] Because so many of the patients that I treat, that I feel like are the most grateful and give me the most soul satisfaction, are some of these women who have been, either they’ve been referred to me or found me somehow because they haven’t been able to find a solution to fix their awful, chronic, horrible problem that they have. And so, over the years now, I’ve had multiple colleagues in town who are experienced gynecologists with patients who have a difficult-to-treat problem that they can’t figure out how to get well, and they’ll send them over to me.
And the truth is, oftentimes, when they send them to me, and I either hear about their history or see the patient before I do anything with them, I think, “This is a hard problem. I’m not sure I can get you better, but I’ll try.”
And like something you said earlier about giving the money back, if you can’t fix somebody, that’s something that I always tell these people that have these problems that are difficult to treat, I’ll tell them, “Look, I don’t know. I think I can help you, but I’m not certain. If I don’t help you, I won’t keep any of your money.”
That helps them feel a lot more comfortable with whatever comes next. But as you’re going over this article, I was thinking about all of the severe conditions in women that I’ve been able to fix with just some PRP.
Charles Runels, MD:
Tell me about one or two that relate to what we’re seeing. Share what you did; maybe someone else will have a similar patient.
Why giving money back when there is no benefit helps you get people well
Before you do that, though, here is just one quick comment about the money-back thing. The other thing that happens, without that understanding and determination to never keep money unless the patient is delighted by what you do, is it blocks you from trying. So if I think I’m going to keep the money, probably, even if they don’t see amazing results, then I would avoid treating them because I’m an ethical person, I don’t want to take their money. So it’s a bit counterintuitive, but you are more likely to take care of some of the hard cases if you’re willing to give back money because you know that you’re not going to steal from them.
They came to get better. So, providing the procedure does not fulfill the promise.
So even if you do the procedure, you don’t keep the money if they’re not delighted.
And that frees you up to take care of some of the harder cases without worrying that someone will be harmed. Because the PRP, of course, is mostly innocuous. And so, you get to proceed and hopefully bail somebody out of something horrible.
Tell us about one or two of your cases that you might think would be instructional, and then we’ll call it a night.
Alexandra Runnels, MD, FACOG:
Sure thing. Yeah, I agree a hundred percent with what you just said. I feel like I can practice much more ethical medicine the way I practice it now than when I was taking insurance. It forces you to be able to be as… When you know somebody’s taking money out of their own pocket to give it to you, you order what is necessary, and you do what you think is going to work, not what somebody on the phone at the insurance company is telling you that you can or can’t order, or whatever.
You end up doing what you think is best for the patient, which is much easier than taking insurance.
A Chronic, Non-Healing, Vaginal Wound
Anyway, that’s a different topic. But as far as some of these kinds of cases, what came to mind is that I was thinking about having one patient who was a forty-something-year-old woman.
She had been seeing another gynecologist with a six-month history of this chronic non-healing wound in her vagina. It was in the posterior fornix of her vagina. It was about a two-centimeter-long defect and about half a centimeter deep that was friable.
And it would bleed.
And it would bleed with intercourse.
And she also had some other pelvic symptoms. She had some IC symptoms and some dyspareunia symptoms.
But the main problem was this chronic non-healing wound inside her vagina, which was something that I had never seen before.
And everything was negative. She didn’t have any… The culture didn’t grow anything interesting. She had no fungus, and the biopsy was negative for any malignancy. It wasn’t anything dangerous or worrisome.
It just would not heal.
And it was a huge worry and a huge problem for her.
They gave her topical estrogen, antibiotic, and antifungal creams for six months. Then somebody tried to cauterize it with silver nitrate and Monsel solution.
And I can’t remember anything else that was tried on her before she came to me, but none of that worked.
She was just beside herself.
And so, I saw her and said, “Well, I think I can probably help you with the IC symptoms with an O-Shot®. And PRP is great at healing up non-healing wounds. I don’t see why it shouldn’t help here. It’s not going to hurt anything.”
So I did a regular O-Shot® on her and then injected about 1 to 2 cc’s of PRP directly into that wound, inside the vagina.
I re-biopsied that moment when I saw it because I thought it looked so bizarre.
Anyhow, two weeks later, she came back for a follow-up, and she said she had not had any symptoms for over a week of any bleeding or any unusual discomfort.
And when I looked inside her vagina, there was no evidence of anything ever even being amiss in there.
And it was previously a 2 by 1.5 centimeter defect that was like granulomatous tissue, that was bleeding. It looked like cancer, it looked like infection. It was just horrible looking. And in two weeks time, it was completely gone. After six months of trying everything else that was available.
And I was amazed, and she was amazed.
And I’ve seen her since, it never came back.
And that’s the kind of thing that happens kind of frequently. There’s lots of other stories, but there’s another story that comes to mind about… I think there was a vaginal stenosis in this article. Is that right?
Charles Runels, MD:
Yes. Before, I wanted to hear that story, too, but was there any hint—maybe I missed it—about what caused her…
Alexandra Runnels, MD, FACOG:
No, no. It was a spontaneously occurring event. It started after having sex one night. So it must have been some trauma from some kind of… It must have been some pretty good sex, I don’t know. But it was after-
Charles Runels, MD:
We’d better move on to the stenosis story, then. Well, maybe let’s leave it right there. Go to the-
Alexandra Runnels, MD, FACOG:
My guess is she’s got some kind of underlying connective tissue disorder, is what I think—made it easier to happen.
Long-Standing Severe Virginal Stenosis and Shortening of the Vagina Post Hysterectomy
But the stenosis story is a woman; she’s in her 60s or so, and she had had a hysterectomy in the past. She was widowed and had not had a sexual partner since her hysterectomy.
That was several years before. She was not on any hormones, but she had lost a bunch of weight. And she was starting her life back over. And she really wanted to be able to have a full life, and she wanted to enjoy sex again and have sex.
One of the problems that she had was her hysterectomy had left her with a very short vagina.
That was because too much of the vaginal vault had been taken at the time of hysterectomy. And so, the length of her vagina was only… I could only put my finger up to about my second knuckle, which was the entire length of her vagina. And she wanted to be able to accommodate a penis.
She had tried. She had had some dates, and she had tried, but she had not been able to accomplish actual penis-in-vagina intercourse despite several attempts since she had had the hysterectomy. And she really wanted that fixed.
So, the surgeon who sent her to me said that his only option was going to be a neo-vagina reconstructed out of some type of graft tissue, which never ends up being anything very functional. It’s usually sad kind of repair, actually.
Or not repair, construction.
But I said, “I don’t know if I can do anything for you, but I’ll try.”
And she wasn’t on any hormones, so I did what I usually do with getting her hormones on board. And then I gave her regular old O-Shot®.
That’s all I did: regular O-Shot® and some hormones.
I said, “I think this is going to take a few rounds of PRP and O-Shots®. And it might take several rounds of hormone pellets. And I’m not sure what else, but vaginal dilators for sure. Topical hormone therapies. I don’t know how long it’s going to take.”
But I had her prepared for a good year working on this project.
When she came back in three months later, she was there for her second round of pellets. Our plan was to do an O-Shot® the first time, which we did. And then a second O-Shot® when she came back three months later.
When she came back at three months, she said, “I don’t need that O-Shot®, but I will take those pellets.”
And I said, “Okay, what do you mean you don’t need the O-Shot®?”
She says, “Well, I made a friend and went on a date. And he has a generous size penis, and I was able to accommodate that penis. Not just accommodate it, but I had two amazing orgasms and had it all night.”
And I said, “I don’t even believe you.”
I didn’t even believe it.
Next Hands-On Workshops with Live Models
So, when I examined her, it was true. Within three months, she had literally grown a vagina long enough to accommodate a very generous penis and have very comfortable, satisfying intercourse. And all it took was an O-Shot® and some pellets.
Charles Runels, MD:
You didn’t even use a dilator or a vibrator or anything?
Alexandra Runnels, MD, FACOG:
I talked to her about it, and she planned on doing it. She just hadn’t done it yet.
Charles Runels, MD:
Interesting.
Alexandra Runnels, MD, FACOG:
Yeah, she never even did it. She met him at the grocery store.
Charles Runels, MD:
Well, that’s very encouraging. I know you got your girls tonight, so thank you for jumping on the call. Let me see if there are any other questions, and then we’ll call it a night.
Stay there, Alex, if I need you to help me answer one. Let’s see. Oh, Heidi Madcap said thank you.
Alexandra Runnels, MD, FACOG:
You’re welcome. Thank you, Heidi.
Charles Runels, MD:
Oh, wow.
Eric has a good story. I’m going to unmute you, Eric, if you don’t mind. If you don’t want to talk, that’s okay. If you can, that sounds interesting. I’d like to hear more about that. Let’s see. I’m trying. Hold on.
Can you hear me?
Post-partum, Chronic Fecal Incontinence made better with PRP
Charles Runels, MD:
Yeah, that sounds fascinating. Tell us what happened.
Eric Byman, MD:
Yeah, this was a woman; I think she was 40 or 42 when she had her first and only child. And she, from the time she gave birth, had fecal incontinence.
This impacted her life because she’d been a long-distance runner, and she couldn’t even make it around the block without jumping back home and jumping on the toilet. It was very life-changing for her.
This went on for a couple of years. We sent her to a pelvic floor PT, but it didn’t really help.
And then I just kind of thought, we’ll try a Hail Mary here.
I told her, “I’m not even going to charge you. Because you got to understand this is completely experimental.”
I made her sign a lengthy, informed consent form that said, “Yeah, I know this is experimental, and there’s no guarantee, and who knows what could happen.”
Then I lost touch with her for a while, and I thought, “Oh, gosh, no follow-up. Who knows what happened.”
But then, when I saw her for her next annual physical, she did come in, and she said, “Oh, yeah, I’m 90% better.”
Charles Runels, MD:
Wow.
Eric Byman, MD:
I ended up using, I think it was 4 mls of PRP, and I just injected half an mL into eight little different spots, circumferentially around the anus, into the anal sphincter itself.
And it clearly worked. She wasn’t a hundred percent better, but it was at the point that she’s almost back to a normal life now.
Charles Runels, MD:
So encouraging.
Thank you for jumping on and telling that story. The thing that we frequently bring up on these calls is the idea that if you’re a $20 million a year quarterback or baseball pitcher and you hurt the muscle of your thigh, you’re going to get PRP. That’s just what’s going to happen because the sports medicine literature is full of how it strengthens the muscle.[29] [30] [31] [32]
It activates the cells that amount to pluripotent stem cells in the area, and remodels fibrosis, so the muscle becomes stronger and less scarred.
Why is that slow to be brought over to mothers?
You can deliver the baby for the NFL football player and not get the same treatment for your pelvic floor or your anus or urinary sphincter that he gets for his thigh muscle.
I’m hoping with studies coming out and enough of us spreading the word, if nothing else, by patient demand, it will become more widely used.
Eric Byman, MD:
If I wanted to write that case up, do you think that a reasonably respected journal would publish it?
Charles Runels, MD:
You know what? I’ll put that in the next email that goes out.
In the little town where I live, we have a fair number of prominent authors who just come here to hide, like Rick Bragg, who won the Pulitzer Prize, Winston Groom, who wrote Forrest Gump, and others.
One of them told me, “Don’t even think about looking for a publisher until someone offers you six figures for something. Just self-publish everything.”
And to me, that’s what you’re looking at with an open-source journal. It’s still peer-reviewed, but you skip all the very long delays and the hassle of going for something that will frustrate you with both peer review and political bias.
So, I’d write it up your patient’s result as a case report for one of the open-source journals. You’ll have it out in six weeks, and we’ll talk about it in one of our Journal Clubs.
Eric Byman, MD:
Can I throw out a little thought I had when I did this procedure?
Charles Runels, MD:
Yes, please.
Eric Byman, MD:
So you know, of course, when we’re doing the O-Shot®, we apply topical BLT cream, then I sometimes apply ice. Well, it occurred to me it’s kind of hard to apply ice to the anal sphincter. And then I thought, why don’t I pour water into a pair of exam gloves, stick it in the freezer, and then use one of those frozen fingers, lubed up, to numb it. And it worked.
Charles Runels, MD:
Very cool. That is a very cool idea. Wow. Yeah, that should go into your case report. It’s so creative and yet obviously effective. That’s a very clever idea. Hey, Alex, are you still there?
Alexandra Runnels, MD, FACOG:
I am.
Charles Runels, MD:
Any comments about Dr. Byman’s-?
Alexandra Runnels, MD, FACOG:
I love the glove in the freezer and the frozen finger. That’s wonderful.
Charles Runels, MD:
You’ll be trying that tomorrow morning.
Alexandra Runnels, MD, FACOG:
I will. I’ll freeze one tomorrow morning.
Charles Runels, MD:
On your own self, after a run or something.
Alexandra Runnels, MD, FACOG:
Stop it.
Charles Runels, MD:
I’m trying to keep it under an hour, Alex, so let’s save your story for next week. But thank you very much for jumping on.
Thank you, Eric. And do text me because I get those occasional emails where they’re asking for case reports, and I’ll shoot you a couple of possibilities.
So many smart people; it’s always an honor. Have a good night. Bye-bye.
References
Alves, Rubina, and Ramon Grimalt. “A Review of Platelet-Rich Plasma: History, Biology, Mechanism of Action, and Classification.” Skin Appendage Disorders 4, no. 1 (January 2018): 18–24. https://doi.org/10.1159/000477353.
Asghar, Aneela, Zahid Tahir, Aisha Ghias, Usma Iftikhar, and Tahir Jameel Ahmad. “Efficacy and Safety of Intralesional Normal Saline in Atrophic Acne Scars.” Annals of King Edward Medical University 25, no. 2 (June 24, 2019). https://doi.org/10.21649/akemu.v25i2.2867.
Bernuzzi, Gino, Federica Petraglia, Martina Francesca Pedrini, Massimo De Filippo, Francesco Pogliacomi, Michele Arcangelo Verdano, and Cosimo Costantino. “Use of Platelet-Rich Plasma in the Care of Sports Injuries: Our Experience with Ultrasound-Guided Injection.” Blood Transfusion 12, no. Suppl 1 (January 2014): s229–34. https://doi.org/10.2450/2013.0293-12.
Brandeis, J, S Lu, R Malik, and C Runels. “(130) Increasing Penile Length and Girth in Healthy Men Using a Novel Protocol: The P-Long Study.” The Journal of Sexual Medicine 20, no. Supplement_1 (May 22, 2023): qdad060.125. https://doi.org/10.1093/jsxmed/qdad060.125.
Bubnov, Rostyslav, Viacheslav Yevseenko, and Igor Semeniv. “Ultrasound Guided Injections of Platelets Rich Plasma for Muscle Injury in Professional Athletes. Comparative Study.,” n.d., 5.
Cass, Shane P. “Ultrasound-Guided Nerve Hydrodissection: What Is It? A Review of the Literature” 15, no. 1 (2016): 3.
“Clinical Benefit of Intra-Articular Saline as a Comparator in Clinical Trials of Knee Osteoarthritis Treatments_ A Systematic Review and Meta-Analysis of Randomized Trials | Elsevier Enhanced Reader.” Accessed April 6, 2022. https://doi.org/10.1016/j.semarthrit.2016.04.003.
El-Amawy, Heba Saed, and Sameh Magdy Sarsik. “Saline in Dermatology: A Literature Review.” Journal of Cosmetic Dermatology 20, no. 7 (2021): 2040–51. https://doi.org/10.1111/jocd.13813.
Fossati, Chiara, Filippo M. N. Randelli, Fabio Sciancalepore, Daniela Maglione, Stefano Pasqualotto, Federico Ambrogi, and Alessandra Menon. “Efficacy of Intra-Articular Injection of Combined Platelet-Rich-Plasma (PRP) and Hyaluronic Acid (HA) in Knee Degenerative Joint Disease: A Prospective, Randomized, Double-Blind Clinical Trial.” Archives of Orthopaedic and Trauma Surgery, October 5, 2024. https://doi.org/10.1007/s00402-024-05603-z.
Geelhoed, Jeannette P., Olivier Wegelin, Ellen Tromp, Bert‐Jan De Boer, Igle‐Jan De Jong, and Jack J. H. Beck. “Improvement in the Ability to Have Sex in Patients with Peyronie’s Disease Treated with Collagenase Clostridium histolyticum .” BJUI Compass 4, no. 1 (January 2023): 66–73. https://doi.org/10.1002/bco2.185.
Hamilton, Bruce, Johannes L. Tol, Wade Knez, and Hakim Chalabi. “Exercise and the Platelet Activator Calcium Chloride Both Influence the Growth Factor Content of Platelet-Rich Plasma (PRP): Overlooked Biochemical Factors That Could Influence PRP Treatment.” British Journal of Sports Medicine 49, no. 14 (July 1, 2015): 957–60. https://doi.org/10.1136/bjsports-2012-091916.
Harrison, P., and the Subcommittee on Platelet Physiology. “The Use of Platelets in Regenerative Medicine and Proposal for a New Classification System: Guidance from the SSC of the ISTH.” Journal of Thrombosis and Haemostasis 16, no. 9 (2018): 1895–1900. https://doi.org/10.1111/jth.14223.
Lin, Haocheng, and Run Wang. “The Science of Vacuum Erectile Device in Penile Rehabilitation after Radical Prostatectomy.” Translational Andrology and Urology 2, no. 1 (2013).
Middleton, Kellie K, Victor Barro, Bart Muller, Satosha Terada, and Freddie H Fu. “Evaluation of the Effects of Platelet-Rich Plasma (PRP) Therapy Involved in the Healing of Sports-Related Soft Tissue Injuries.” The Iowa Orthopaedic Journal 32 (2012): 150–63. http://www.ncbi.nlm.nih.gov/pubmed/23576936.
Moraes, Vinícius Y, Mário Lenza, Marcel Jun Tamaoki, Flávio Faloppa, and João Carlos Belloti. “Platelet-Rich Therapies for Musculoskeletal Soft Tissue Injuries.” The Cochrane Database of Systematic Reviews 12 (January 2013): CD010071. https://doi.org/10.1002/14651858.CD010071.pub2.
Ng, Jun Jiet, Sukanda Jaili, John Yen Sing Lee, Nur Ain Yaakob, and Vaitheswariy Rao Nalathambi. “Platelet-Rich Plasma in Urogynecology: A Case Series.” Cureus 16, no. 8: e68004. Accessed October 8, 2024. https://doi.org/10.7759/cureus.68004.
Ragheb, Ahmed M., Amr M. Lotfy, Mohamed Fahmy, and Akrm A. Elmarakbi. “Safety and Efficacy of Platelet-Rich Plasma Injection for Treatment of Erectile Dysfunction: A Prospective Randomized Controlled Study.” Basic and Clinical Andrology 34, no. 1 (October 8, 2024): 16. https://doi.org/10.1186/s12610-024-00232-3.
Roohaninasab, Masoumeh, Alireza Jafarzadeh, Afsaneh Sadeghzadeh‐Bazargan, Sona Zare, Maryam Nouri, Mohammad Ali Nilforoushzadeh, and Elham Behrangi. “Evaluation of the Efficacy, Safety and Satisfaction Rates of Platelet‐rich Plasma, Non‐cross‐linked Hyaluronic Acid and the Combination of Platelet‐rich Plasma and Non‐cross‐linked Hyaluronic Acid in Patients with Burn Scars Treated with Fractional CO2 Laser: A Randomized Controlled Clinical Trial.” International Wound Journal 21, no. 10 (October 2, 2024): e70065. https://doi.org/10.1111/iwj.70065.
Rossi, Luciano, Maximiliano Ranalletta, Ignacio Pasqualini, Juan Pablo Zicaro, Matías Costa Paz, Pablo Camino, and Nicolas S. Piuzzi. “Substantial Variability in Platelet-Rich Plasma Composition Is Based on Patient Age and Baseline Platelet Count.” Arthroscopy, Sports Medicine, and Rehabilitation 5, no. 3 (May 20, 2023): e853–58. https://doi.org/10.1016/j.asmr.2023.03.017.
Saltzman, Bryan M., Timothy Leroux, Maximilian A. Meyer, Bryce A. Basques, Jaskarndip Chahal, Bernard R. Bach, Adam B. Yanke, and Brian J. Cole. “The Therapeutic Effect of Intra-Articular Normal Saline Injections for Knee Osteoarthritis: A Meta-Analysis of Evidence Level 1 Studies.” The American Journal of Sports Medicine 45, no. 11 (September 1, 2017): 2647–53. https://doi.org/10.1177/0363546516680607.
Sclafani, Anthony P., and Steven A. McCormick. “Induction of Dermal Collagenesis, Angiogenesis, and Adipogenesis in Human Skin by Injection of Platelet-Rich Fibrin Matrix.” Archives of Facial Plastic Surgery 14, no. 2 (April 2012): 132–36. https://doi.org/10.1001/archfacial.2011.784.
Sheean, Andrew J., Adam W. Anz, and James P. Bradley. “Platelet-Rich Plasma: Fundamentals and Clinical Applications.” Arthroscopy: The Journal of Arthroscopic & Related Surgery 37, no. 9 (September 2021): 2732–34. https://doi.org/10.1016/j.arthro.2021.07.003.
Twisy, Howida Omar. “Subcision with Platelet-Rich Plasma and Microneedling versus Subcision with Saline and Micro-Needling in Posttraumatic Scars.” Archives of Dermatological Research 316, no. 8 (August 19, 2024): 537. https://doi.org/10.1007/s00403-024-03226-3.
Wang, Run. “Is There Still a Role for Vacuum Erection Devices in Contemporary Sexual Medicine?” The Journal of Sexual Medicine 19, no. 5 (May 1, 2022): 682–85. https://doi.org/10.1016/j.jsxm.2022.02.013.
Welliver, R. Charles, Clay Mechlin, Brianne Goodwin, Joseph P. Alukal, and Andrew R. McCullough. “A Pilot Study to Determine Penile Oxygen Saturation Before and After Vacuum Therapy in Patients with Erectile Dysfunction After Radical Prostatectomy.” The Journal of Sexual Medicine 11, no. 4 (April 1, 2014): 1071–77. https://doi.org/10.1111/jsm.12445.
Wikramanayake, Tongyu C., Nicole I. Haberland, Aysun Akhundlu, Andrea Laboy Nieves, and Mariya Miteva. “Prevention and Treatment of Chemotherapy-Induced Alopecia: What Is Available and What Is Coming?” Current Oncology 30, no. 4 (March 25, 2023): 3609–26. https://doi.org/10.3390/curroncol30040275.
Yogiswara, Niwanda, Fikri Rizaldi, and Mohammad Ayodhia Soebadi. “The Potential Role of Intracavernosal Injection of Platelet-Rich Plasma for Treating Patients with Mild to Moderate Erectile Dysfunction: A GRADE-Assessed Systematic Review and Meta-Analysis of Randomized Controlled Trials.” Archivio Italiano Di Urologia e Andrologia 96, no. 3 (October 2, 2024). https://doi.org/10.4081/aiua.2024.12687.
Helpful Links
=> Next Hands-On Workshops with Live Models <=
=> Dr. Runels Botulinum Blastoff Course <=
=> The Cellular Medicine Association (who we are) <=
=> Apply for Online Training for Multiple PRP Procedures <=
=> FSFI Online Administrator and Calculator <=
=> 5-Notes Expert System for Doctors <=
=> Help with Logging into Membership Websites <=
=> The software I use to send emails: ONTRAPORT (free trial) <=
=> Sell O-Shot® products: You make 10% with links you place; shipped by the manufacturer), this explains and here’s where to apply <=
[1] Ragheb et al., “Safety and Efficacy of Platelet-Rich Plasma Injection for Treatment of Erectile Dysfunction.”
[2] Asghar et al., “Efficacy and Safety of Intralesional Normal Saline in Atrophic Acne Scars.”
[3] Cass, “Ultrasound-Guided Nerve Hydrodissection: What Is It? A Review of the Literature.”
[4] El-Amawy and Sarsik, “Saline in Dermatology.”
[5] Saltzman et al., “The Therapeutic Effect of Intra-Articular Normal Saline Injections for Knee Osteoarthritis.”
[6] “Clinical Benefit of Intra-Articular Saline as a Comparator in Clinical Trials of Knee Osteoarthritis Treatments_ A Systematic Review and Meta-Analysis of Randomized Trials | Elsevier Enhanced Reader.”
[7] Ragheb et al., “Safety and Efficacy of Platelet-Rich Plasma Injection for Treatment of Erectile Dysfunction.”
[8] Yogiswara, Rizaldi, and Soebadi, “The Potential Role of Intracavernosal Injection of Platelet-Rich Plasma for Treating Patients with Mild to Moderate Erectile Dysfunction.”
[9] Brandeis et al., “(130) Increasing Penile Length and Girth in Healthy Men Using a Novel Protocol.”
[10] Geelhoed et al., “Improvement in the Ability to Have Sex in Patients with Peyronie’s Disease Treated with Collagenase <span Style=”font-Variant.”
[11] Lin and Wang, “The Science of Vacuum Erectile Device in Penile Rehabilitation after Radical Prostatectomy.”
[12] Wang, “Is There Still a Role for Vacuum Erection Devices in Contemporary Sexual Medicine?”
[13] Welliver et al., “A Pilot Study to Determine Penile Oxygen Saturation Before and After Vacuum Therapy in Patients with Erectile Dysfunction After Radical Prostatectomy.”
[14] Yogiswara, Rizaldi, and Soebadi, “The Potential Role of Intracavernosal Injection of Platelet-Rich Plasma for Treating Patients with Mild to Moderate Erectile Dysfunction.”
[15] Ragheb et al., “Safety and Efficacy of Platelet-Rich Plasma Injection for Treatment of Erectile Dysfunction.”
[16] Yogiswara, Rizaldi, and Soebadi, “The Potential Role of Intracavernosal Injection of Platelet-Rich Plasma for Treating Patients with Mild to Moderate Erectile Dysfunction.”
[17] Twisy, “Subcision with Platelet-Rich Plasma and Microneedling versus Subcision with Saline and Micro-Needling in Posttraumatic Scars.”
[18] Roohaninasab et al., “Evaluation of the Efficacy, Safety and Satisfaction Rates of Platelet‐rich Plasma, Non‐cross‐linked Hyaluronic Acid and the Combination of Platelet‐rich Plasma and Non‐cross‐linked Hyaluronic Acid in Patients with Burn Scars Treated with Fractional CO2 Laser.”
[19] Fossati et al., “Efficacy of Intra-Articular Injection of Combined Platelet-Rich-Plasma (PRP) and Hyaluronic Acid (HA) in Knee Degenerative Joint Disease.”
[20] Ng et al., “Platelet-Rich Plasma in Urogynecology.”
[21] Rossi et al., “Substantial Variability in Platelet-Rich Plasma Composition Is Based on Patient Age and Baseline Platelet Count.”
[22] Harrison and Physiology, “The Use of Platelets in Regenerative Medicine and Proposal for a New Classification System.”
[23] Hamilton et al., “Exercise and the Platelet Activator Calcium Chloride Both Influence the Growth Factor Content of Platelet-Rich Plasma (PRP).”
[24] Sheean, Anz, and Bradley, “Platelet-Rich Plasma.”
[25] Alves and Grimalt, “A Review of Platelet-Rich Plasma.”
[26] Wikramanayake et al., “Prevention and Treatment of Chemotherapy-Induced Alopecia.”
[27] Sclafani and McCormick, “Induction of Dermal Collagenesis, Angiogenesis, and Adipogenesis in Human Skin by Injection of Platelet-Rich Fibrin Matrix.”
[28] Ng et al., “Platelet-Rich Plasma in Urogynecology.”
[29] Bernuzzi et al., “Use of Platelet-Rich Plasma in the Care of Sports Injuries.”
[30] Bubnov, Yevseenko, and Semeniv, “Ultrasound Guided Injections of Platelets Rich Plasma for Muscle Injury in Professional Athletes. Comparative Study.”
[31] Middleton et al., “Evaluation of the Effects of Platelet-Rich Plasma (PRP) Therapy Involved in the Healing of Sports-Related Soft Tissue Injuries.”
[32] Moraes et al., “Platelet-Rich Therapies for Musculoskeletal Soft Tissue Injuries.”

It’s great to see ongoing research and discussion around the effectiveness of PRP and the P-Shot® for men’s sexual health,…