|
Journal Club with Pearls & Marketing 2024.07.16 Cellular Medicine Association |
JCPM2024.07.16
The following is an edited transcript of the Journal Club with Pearls & Marketing (JCPM) of July 16, 2024, with Charles Runels, MD.
-> The pdf of this live journal club can be downloaded here <-<
Topics Covered
- One Research Paper Shows PRP Injected Does Not Help Urinary Incontinence in Women: What Went Wrong?
- A Sampling of Studies Showing that Injected PRP Does Help Women with Urinary Incontinence
- Wrong Assumptions that Could Decrease Effectiveness of Your O-Shot® Procedure
- Error: Using saline as a placebo in a regenerative study.
- Error: Injecting too proximal to the bladder
- Error: Treating the wrong person (patient selection)
- Error: Injecting too deep in relation to the vaginal wall
- Error: Not Activating the PRP
- Error: Making PRP with a lab centrifuge and tube made for analysis (not for preparing PRP to be reinjected back into the body)
- Error: Heating the PRP
- Error: Using PRF instead of PRP to do an O-Shot® procedure
- Error: Thinking everyone should see results after only one procedure
- Error: Not gladly refunding all the money or repeating the procedure if the patient is not thrilled with the results
- Error: Not injecting the clitoris when treating incontinence
- Error: Not Appreciating the Angle of the Urethra (and modifying your injection accordingly)

Charles Runels, MD
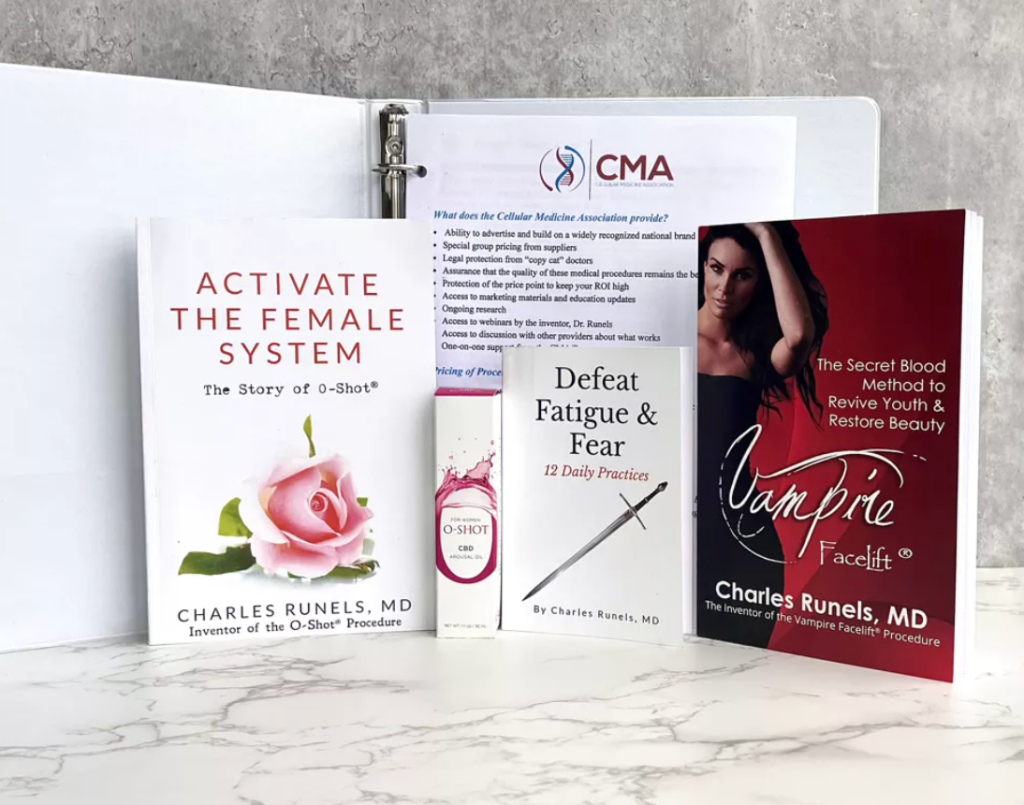
Author, researcher, and inventor of the Vampire Facelift®, Orchid Shot® (O-Shot®), Priapus Shot® (P-Shot®), Priapus Toxin®, Vampire Breast Lift®, and Vampire Wing Lift®, & Clitoxin® procedures.
Transcript
Welcome to the journal club.
One Research Paper Shows PRP Injected Does Not Help Urinary Incontinence in Women—What Went Wrong?
There is a new article about using platelet-rich plasma for urinary incontinence in women,[1] and there’s an editorial about it,[2] so I wanted to review it.
It relates to a text message I received today. The question said, “I treated someone with the O-Shot® for incontinence, and it got better for a couple of weeks, and then it came back. What should I do?”
And I think it’s timely that she asked the question because this research just came out this month, so let’s review it.
Here’s the editorial comment. It’s in the Gold Journal, and the conclusion was that at least the way this was done did not work or did not do better than placebo. They used this study; let’s pull that one up for you.
The method was a single-blinded, randomized, placebo-controlled trial, single location, demonstrable stress, predominant urinary incontinence, and they randomized either five CCs of PRP or saline at the anterior vaginal wall at the urethra and the primary outcome was how dry they were at six months.
The negative stress cough tests answered much better, very much better, or not so much.
So, 50 patients were enrolled, and they found no statistical difference between the two groups. No major side effects. And lack of side effects is not surprising considering our experience with the O-Shot® procedure, but their conclusion of no benefit is surprising because they say at this time, there’s insufficient evidence to offer a one-time PRP injection into the anterior vaginal wall for the treatment of female stress urinary incontinence.[3]
There are a couple of things about this.
First, just because the way you did it shows that it didn’t work doesn’t mean all the previous studies that show that it does work are wrong.[4] [5] [6] [7] [8] [9]
So you see the jump they made?
We did it mid-urethra, and it didn’t work. So, there’s insufficient evidence because our method didn’t work. The unexplained assumption in that statement is that no matter where you inject it or how you prepare the platelet-rich plasma, it should be ubiquitously effective across the board, which is wrong.
No matter how many times you inject it or where you inject it, it shouldn’t matter. Otherwise, you wouldn’t be able to say that, at this time, there is insufficient evidence to offer a one-time injection in the anterior vaginal wall because there are other studies.
So, let me show you some of those other studies and explain what they did differently.
They did not use an O-Shot® procedure. When I have people who take our courses both online and in person tell me that they’re not seeing results, most of the time, they are using the procedure the way this study did, and it does not work this way.
A Sampling of Studies Showing that Injected PRP Does Help Women with Urinary Incontinence
So, let’s look at a few studies showing that injecting platelet-rich plasma provides benefits. Let me see if I can tease out the differences between these investigators and what we do.
So here are a few of the studies I’ve pulled. There’s more, but here are a few of my favorites. There are more studies to the same effect that I’m about to show you with interstitial cystitis,[10] [11] [12] mesh,[13] [14] [15], and dyspareunia[16] [17] [18]; there are quite a number of studies.
When I see someone act like there’s nothing written, I always wonder what they’re reading. Are they reading Marvel Comics?
Here are a few of the other studies.
Here’s one that shows benefit, but if you notice the difference, they injected three treatments separated by a month and they showed benefit.[19]
I will show you a different one. In this study, they injected twice (and combined PRP with pelvic floor muscle training) and demonstrated that it effectively relieved stress-related incontinence with a high success rate.[20]
In the first study that we published, regarding our O-Shot® and sexual function, the second person who I treated told me that she was running again because it had helped her incontinence.[21]
I hadn’t anticipated the improvement in SUI (I was looking for the sexual response), but she reported that she was able to run again. However, the primary endpoint of the study was sexual dysfunction, and we showed it helped (with improvement on the female sexual distress scale).
Not surprisingly, in our study of the Clitoxin® procedure, by affecting the autonomic nervous system, injecting botulinum toxin into the clitoris alone (not the anterior vaginal wall) also helped with stress and urge incontinence.[22]
Wrong Assumptions
Let me see if I can provide an overview of why there are some misunderstandings and, I think, wrong assumptions.
This study, I think, makes one of our points. If you look at this study, we showed effective results (with two blinded dermatopathologists) demonstrating the effect of injecting platelet-rich plasma for lichen sclerosus.[23]
Also, in this study, one of the gynecologists in our group (Kathleen Posey, MD, FACOG) showed that PRP improved the results when surgically treating phimosis secondary to lichen sclerosus.[24]
Error: Using Saline as a Placebo in a Regenerative Study
Then, in this study, they used a saline placebo; in that study, 50% of the placebo arm improved on biopsy. So, because the placebo arm was 50% effective, the treatment arm wasn’t much different.
But show me another study with lichen sclerosus where 50% of the placebo arm improves on biopsy. You won’t find one.
And we’ve gone over multiple times here in our journal club that saline injected IV, compared to morphine, is a placebo. But when you’re hydrodissecting tissue with saline, that is not a placebo, which is well-supported in the dermatology literature.
I’ll show you some of those studies where saline is used to treat scars, leishmaniasis, and even degenerative joint disease.[25]
Here’s a review article about using saline in dermatology to treat problems. You can see it’s been used for because you’re lifting the skin away and hydrodissecting; there’s a benefit to it.
Here’s another one, a literature review of using saline as a treatment, a helpful option, intralesional injections as a therapeutic option, and saline for joints.[26] There’s atrophic scars,[27] improvement in hernioplasty.[28].
So when I see a study comparing platelet-rich plasma hydrodissecting tissue and the anterior vaginal wall compared with saline, I don’t think that the investigators are not smart. I think they’re unaware that there is a strong and undeniable body of literature in the dermatology side that shows that that is not a placebo.
So, the first thing that’s wrong with this study is that their placebo was not a placebo.
Error: Injecting too proximal to the bladder
The second thing that makes it not a legitimate criticism of our O-Shot® procedure is the location of the injection. If part of the procedure is hydrodissection, it matters where you put the needle, both the location along the urethra and the depth of the insertion site.
Over and over again for the past 14 years, having trained hundreds of physicians, I hear that, especially in the gynecology world where, of course, they know the anatomy better than I do, they’re dissecting it every day, but they go home and say, “Yes, you’re right.”
“Classically, we were trained to inject bulking materials (like Coaptite® and collagen) mid-urethra or near the ureterovesical junction, but the O-Shot® works better when injected near the introitus, literally half a millimeter or less on the other side of the hymenal remnant.”
And the first one or two rugae that you see when you look inside the vagina. Any deeper and your effectiveness is decreased.
To figure out why, we need to do some visual studies with MRI and ultrasound. But if you go further, more proximal to the bladder, you are not doing an O-Shot®; you’re doing something different.
My theory about why that’s happening is that if you study Delancey’s work, especially what he’s published from cadaver studies,[29] [30] [31] the layers of the urinary sphincter are such that they abut the muscle of the vaginal wall near the introitus and there only becomes a space as you go closer to the bladder, more proximal to the bladder.
So I think what’s happening is that when you inject closer to the introitus, you may be injecting the muscles of the urinary sphincter. When you go near the ureterovesical junction more proximal to the bladder, there’s a space there.
And I used to think that perhaps we were hydrodissecting that space and causing neovascularization, collagenesis, that was bulking, causing our effectiveness with stress incontinence.
But now we’ve had more than a decade of experience showing that it doesn’t work so well when you go more proximal to the bladder. We have a stack of literature showing that when you inject the muscles (in the sports medicine literature), you activate what amounts to pluripotent stem cells, strengthen the muscle by activating myocyte formation, and help remodel scar tissue so there’s less fibrosis and more active muscle.[32] [33] [34] [35] [36] [37]
So, if you’re a quarterback for the NFL and injure your thigh muscle, you will be injected with a platelet-rich plasma. And, of course, that level of acceptance hasn’t bled over into repairing your wife or your mother’s urinary sphincter muscles postpartum or post-menopause as those muscles become weaker, but it’s still muscle.
So, let’s say it out loud: If you are a quarterback for the NFL, your thigh muscles may receive better treatment than your urinary sphincter muscles if you are a woman.
With the urinary sphincter, you have smooth muscle, and of course, you have somatic muscle there as well. And that’s my theory. We would need ultrasound studies. I guess you’d need cadaver studies. I’m not sure what it would take to prove that, but I know this study that showed no benefit to injecting PRP into the mid-urethra was not an O-Shot®.
I’ll give you a list of other things that were different about it, then what we do, and some pearls both in how to do the procedure and the politics and economics of how to do this so that your patients are happy, you have a very high success rate, most of your people are helped. None of them go away feeling like you took advantage of them.
Okay, so first, we have many people in our group who claim—I even have trouble saying it—they get 100% effectiveness using our O-Shot® procedure for incontinence, but they’re not treating 100% of the people who show up.
Error: Treating the wrong person (patient selection)
So, part of assuring success is patient selection, just like with any other procedure.
The woman being treated should not have a significant cystocele. You can still perform the procedure, and sometimes, you will see results. However, your success rate will go down.
We now have people in our group who have been doing the O-Shot® procedure, me included, for over a decade with a high success rate.
So there are many more studies out there—not hundreds, but another half a dozen, depending on how you want to count them—showing benefits, but they’re not doing it the way you just saw.
The location of the injection along the urethra matters. And the woman’s anatomy matters (co-morbidities).
Error: Injecting too deep in relation to the vaginal wall
Also, when I’m teaching people this procedure, they tend to go too deep with the needle (in relation to the surface of the vagina).
Even when I warn them, almost without exception, people go too deep. When doing this procedure, you are too deep if you’re more than three millimeters deep, five millimeters max.
This is a subdermal injection.
If you were suturing the skin or the surface of the intervaginal wall, going more than a millimeter or two deeper than where you would go with your needle to repair the surface layer, you’re too deep.
The other thing is that as people press on the plunger, they tend to advance the needle as they advance the plunger (completely unaware) while I’m telling them they’re advancing the needle.
They’re more focused on where the needle is inserted than on how deep it goes. But there’s an almost universal tendency to advance the needle as you’re injecting, and that most definitely decreases the effectiveness of the procedure.
Now, I’ll stop here for a second.
I haven’t done a split study with three different levels of injection and three different locations, but one of the studies that showed benefit, they injected three different locations, and one of the locations is where we have found the most benefit, which is just the other side of the introitus, of the hymenal remnant. If you’re looking at the anterior vaginal wall, when you start to see those horizontal rugae, it’s smooth around the heart’s line. It’s shiny and smooth, and the way you know you’re inside of the vagina, you start to see these horizontal rugae on the anterior vaginal wall.
And when you get to the second or third one, that’s as far in as you need to go.
Error: Not Activating the PRP
It also matters whether you activate the platelet-rich plasma, which they did not in the study we are considering.
I have repeatedly had people tell me that a drug rep who sold them this centrifuge told them they didn’t have to activate it. A stack of the literature shows that you have a different spectrum and a different amount of growth factors when you do not activate with calcium chloride or calcium gluconate so that matters.
The speed at which it goes from PRP to platelet-rich fibrin matrix, which holds it in place, that is different with activation versus non-activation.
While lecturing in Serbia, a scientist there shared the podium with me. He studied platelets for his whole career, 40 years.
And he said, “If you don’t activate with something before injection, you’re only getting 65% activation.”[38] [39] [40] [41] [42] [43]
If your centrifuge is a gel centrifuge and you’re only getting 1.5 times the concentration of whole blood, but then you’re only activating 65% of your supernatant, you might as well have skipped this centrifuge and just injected the whole blood.
So, it matters. And I have had more than one doctor go home from my workshop and say, my results with my O-Shot® aren’t so good.
And then I find out some drug rep has told them, “Oh, you don’t have to activate it.”
You do.
Now, I don’t activate it with the face, but with the face, I like for it to spread, and you get a more field of more of a field effect. Same with the scalp. Even though one study did activate with calcium chloride, I’m looking for a field effect, but when I’m injecting around the urethra, I want it to go in and gel as quickly as possible and stay as local as possible to where I put the needle. So that matters.
Error: Making PRP with a lab centrifuge and tube made for analysis (not for preparing PRP to be reinjected back into the body)
Some people are still trying to make their own PRP without using an FDA-cleared device to prepare PRP to go back into the body. Having watched people do that and imagining someone who just smoked a joint and works for you, they double as the receptionist, and they take your clothes to the cleaner and spin your blood. It’s not going to be consistent if you’re doing a pipette technique, but if you’re doing an FDA-approved gel kit or another kit with a very definite protocol that’s been proven to the FDA that it prepares certain level of platelet-rich plasma and a sterile way to go back into the body, then even if that same person is now preparing your PRP, you’re going to get something consistent.
So, I think that matters, and I don’t think PRF is appropriate for the O-Shot®.
It’s a mess if you want to use it for the O-Shot®.
As a dentist to patch a wound or if you’ve come up with a technique you’re using in the face; I don’t think it matters that much.
Error: Heating the PRP
Also, I see people heating platelet-rich plasma. I think that’s, yeah, you’re making a gel, but in the same way, when you heat an egg, it gels up. But you’re denaturing proteins; those are small amino acids that change that you’re changing their nature.
And I think changing the activity. It might look pretty when you put it in the face, but I think you’ve changed the nature of an amino acid when you cook it. So, I don’t say you don’t do it, but I wouldn’t call it an O-Shot®, and I wouldn’t call it a Vampire Facelift® if you’re using PRF because you’ve changed the nature of the biological bioactive nature of the material, you’re putting in the face.
Error: Using PRF instead of PRP to do an O-Shot® procedure
I know there’s dental literature about using it to patch a wound, but if you’re making a gel with PRF or some heating process, micronizing it, and trying to squirt it through a 30 gauge needle—and you shouldn’t be using anything larger than a 30 gauge needle to do the clitoral injection of an O-Shot® —then you’re not doing an O-Shot®.
 The people who did this study did not do an O-Shot®.
The people who did this study did not do an O-Shot®.
They did something. However, they confirmed that a protocol different from ours did not work.
Error: Thinking everyone should see results after only one procedure
When we survey, we’ve got a survey now that’s got over a thousand people in it, where patients have been surveyed after doing any form of an O-Shot® for any problem. So that’s even the hard-to-treat problems like “anorgasmia for my whole life.”
According to that survey, 65% love it after the first procedure, and 85% love it after you repeat it.
I often see women who have one O-Shot® and their incontinence gets better, and then after the second, no-shot, and I like repeating it eight weeks later, not four because your full effect is eight to 12 weeks.
But a second procedure, an O-Shot® procedure at eight weeks, 85% love it. Even when you’re treating the hard-to-treat problems.
For incontinence, it’s even better.
So, then you think, “Well, why not just give everybody two injections?”
It’s because if you do it correctly, 65% of people love it after the first one.
My practice is that I give them one procedure, and then if they’re not thrilled with it, you call and find out if they’re thrilled with it because some people will decide they don’t like it but never let you know. So, you follow up, and if they’re not thrilled, you bring them back for a repeat procedure or offer them either their money back or something of equal value for free.
Without that, I think you’ll have angry people because they didn’t pay for the procedure. They paid you for the results you promised.
Even though you told them nothing works 100% of the time, this isn’t an insurance-based procedure. If you do something that’s insurance-based and they don’t get the benefit they expected, it doesn’t really hurt them because they’re still paying or their employer’s paying insurance every month, and they’re not out of anything other than their time, and whatever minimal side effect they had with PRP.
But if you promised them an effect from a cash procedure and it doesn’t work, in my opinion, you’re obligated to find out if they feel that promise was fulfilled and, if not, do something until they feel that they were not hurt financially.
Always, if they have an attitude that they still want to be better and they’re not angry or impatient or just in my gut tells me for some reason, this is not a relationship that’s going the right direction because sometimes it can be a family member. The patient wants to keep participating, but their spouse somehow seems adversarial.
This is a once or twice-a-year thing, not once or twice a week when you’re careful about your patient selection, but I’ll end the relationship and give them a complete refund. If otherwise, they’ve been a patient and are happy with me, I help them find another doctor and treatment alternative with a referral to someone else.
But they never, as far as I know, after taking now cash for procedures for the past 21 years, since 2003, really before that, everyone I treated either loved what I did or I don’t have their money—they received a complete refund.
That makes you more careful about patient selection.
And most of our people, as far as I know, I never say always, but what’s supposed to be happening is that everyone in our group follows that same philosophy. We have people doing, O-Shot® now with very happy patients for over a decade.
Those are the rules to follow as far as the finances go.
I don’t like repeating it before eight weeks. Even though in one of those studies, they were going every four, and in most hair studies, people inject every four to six weeks. In the microneedling studies, it’s every four to six weeks. But if you look at the wound care studies, full effect for soft tissue treated with platelet-rich plasma is eight to 12 weeks. So, to me, it feels like you’re wearing them out. You’re wearing yourself out if you don’t wait at least give it eight weeks (which is around the time 80% of the effectiveness recurs) before you repeat it.
This is not a pharmaceutical effect. So, I can give you an anticholinergic orally, which might help your incontinence, but I couldn’t squirt PRP down your throat and expect it to help your incontinence.
It’s an exaggeration, but the same idea applies even to tissue in the area of the vagina. An injection mid-urethra or too deep is not the same as an injection distal urethra and shallow. It’s not the same.
And that’s what they did.
If your O-Shot® is not at least 85% to 95% effective after two injections, you might want to rewatch the videos or do a hands-on workshop with either me or one of our teachers who do see wonderful effects.
We have teachers all over the world now. Not all of them are active all the time, but we have over a hundred doctors who have taught for us, many of them professors at various colleges. They’re teaching it because they’ve seen it work, and we have studies to back it up.
So, one study done in a different way does not negate a decade plus over 2000 doctors in 50 plus countries and a whole stack of other studies showing benefits, but you should know that it’s there and that it makes a difference how you do the procedure.
They showed us that the mid-urethra without activating the PRP does not work as well as the distal urethra injection with activation.
And one injection is not as effective as offering two or three injections, especially if you’re going for the sexual effects.
Error: Not gladly refunding all the money or repeating the procedure if the patient is not thrilled with the results
Don’t offer the procedure unless you’re prepared to return all the money. There’s a name for this. My middle son is a finance guy and deals with millions of dollars in his job. And when you book a plane, I don’t know if you know this, but when you buy a plane ticket with Delta, that money goes into some fund. That’s a buffer fund. They don’t spend it until they deliver the promise of getting your booty from Atlanta to London, Atlanta to LA, or wherever you’re going. It’s because they haven’t fulfilled the promise.
When someone gives me money for an O-Shot®, I consider it not money for me to spend until they tell me, “Yes, my incontinence is gone, or Yes, my dyspareunia is improved. Yes, something is better about my life that I think it’s worth the 1500 dollars” or whatever it was they paid me for the procedure.
I didn’t consider their payment to be my money until they tell me it worked by their definition.
So don’t offer the procedure unless you’re prepared to follow that idea. Just like Delta, it’s not Delta’s money until they get your booty from Atlanta to London if that’s what they promised you, and that O-Shot® money is not yours until their incontinence is improved (if that’s why they underwent the procedure).
Error: Not injecting the clitoris when treating incontinence
The other part that’s significantly different is that I’ve seldom I’ve done it, but I very seldom, probably one out of a hundred O-Shot®’s, do I inject the anterior vaginal wall that I don’t also inject the clitoris (always with nothing larger than a 30-guage needle).
And you think, “Well, why would you inject the clitoris when it’s an incontinence problem?”
We know there’s erectile tissue surrounding the urethra just as there is with the urethra of the male, of the penis.
There is some communication between the erectile tissue of the clitoris and the urethra.
As we showed with our study recently, my wife and I, who did the study with botulinum toxin and PRP in the clitoris for sexual dysfunction, some autonomic processes can go on that happen more likely when you’re injecting the clitoris.[44]
If you look at the neuroanatomy, the autonomic nervous system, just the number of nerves there is much more than somatic. You’ve got the pudendal nerve, which turns into the dorsal nerve of the clitoris, but you also have the autonomic nervous system with the inferior hypogastric plexus and all that goes with that. And that is most likely being affected when you inject the clitoris with PRP.
We know from many studies, tissue studies, wound care studies, and even studies of neurological problems, like anything from the numbness posts associated with diabetes, you get neurogenesis with PRP.
Even in vitro studies, you can grow nerves with PRP.
So, if you consider the nerves of micturition and those that might be associated with urge incontinence, that’s part of the reason I always inject the clitoris.
The other reason is that can we agree that some people lie about sex? I’ve even had women tell me that they told their husbands they were getting the O-Shot® for incontinence, but they were interested in improving the sex, but they didn’t want their husbands to know for fear of hurting his feelings.
In one case, the lady loved her husband and wanted to stay with him, but he was dying of prostate cancer, and she had a boyfriend. It took a lot of courage for her to tell me that. The next woman with that situation may not tell me. So, in less than 1%, do I not inject the clitoris, even if their complaint is incontinence.
And, of course, in this study, they did not inject the clitoris.
A little trick to help
Some of our more thoughtful doctors told me they did the O-Shot®, and when it didn’t work so well, they had the person come back and put in a little in-and-out catheter to more easily visualize where the urethra is.
If you do this injection other than just beneath the urethra, you’re missing the urinary sphincter. If you’re at one or two or nine o’clock or 10 o’clock and not right beneath the urethra at 12 o’clock with the 12 being defined where the urethra is, you’re not doing an O-Shot®.
Error: Not Appreciating the Angle of the Urethra (and modifying your injection accordingly)
The other part is just the angle of the urethra, just like the vaginal wall angles. Some people, of course, when you do your pap smear, you’re looking at the anterior vaginal wall when they’re flat supine, and it might be parallel to the floor or to the wall depending on the tone of the vaginal wall musculature and the pelvic floor and where they have a cystocele.
Appreciating the angle of the urethra and slipping your needle in such that it is not going too deep either into the urethra or past it or either side of it, but hydrodissecting the tissue beneath/anterior to it. And at the most distal part of it, that is the tip.
This is not brain surgery, but it’s not easy and mindless either.
The P-Shot®, I think, is much easier than the O-Shot® procedure. Treating hair with PRP is relatively simple. But I think to do the O-Shot®, you have to not only understand the female anatomy, but you have to be able to look at the vagina and think about what’s going on and understand that woman’s unique anatomy; vaginas are like snowflakes (all beautiful and all different).
I disagree with the artists who say, “We’re doing bad things when we do vaginoplasty because we’re making women feel uncomfortable about their labia.”
I don’t agree with that because some women do feel uncomfortable with their labia. It hangs out of their bathing suit. It hurts when they have sex. On one side, it’s asymmetric, for whatever reason. If you’re a woman, you get to decide if your labia is attractive to you or not. And research shows that when you do labioplasty for a woman who’s bothered by the appearance of her labia, her sexual response improves.[45] [46]
On the other hand, we were all made beautiful. But vaginas can be significantly different, as you know, by the angle and the location of the urethra. And if you can’t look at things and sort out where it’s going and you blindly stick the needle in at any depth, or if you just say, “I’m going to go mid-urethra” without contemplating the things we just talked about as far as depth and what you’re doing with the platelet-rich plasma, you’re doing something but you’re not doing an O-Shot® procedure.
And I think if I were going to summarize all that and say it would be watching the videos at least three or four times. If you’re still not getting results, get a hands-on workshop with one of our teachers. No one teaches our procedures without enough experience to be confident that with a lot of success and knowing those nuances, they’ll be able to watch what you’re doing and correct what may be you’re not aware of.
Usually, I find when I’m teaching this procedure, really brilliant surgeons that could do their complicated procedures for which I don’t even know the names of the tools literally in the dark, but for some reason, when they’re injecting, they may not be aware of what they’re doing with the depth of the needle.
And so having someone who’s done this a lot, watch you do it, could be helpful if you’re not seeing at least 85% success rate after the second procedure.
And I think with that, I will see if there are questions, and if not, we’ll call it a night. Let’s see. Okay, I guess that’s it.
I’ll see you next week. Thank you for showing up. Hopefully, that was helpful.
References
Agarwal, Varsha, Ambika Gupta, Harneet Singh, Mala Kamboj, Harsha Popli, and Suman Saroha. “Comparative Efficacy of Platelet-Rich Plasma and Dry Needling for Management of Trigger Points in Masseter Muscle in Myofascial Pain Syndrome Patients: A Randomized Controlled Trial.” Journal of Oral & Facial Pain and Headache, November 28, 2022. https://doi.org/10.11607/ofph.3188.
Alavi-Arjas, Fatemeh, Michael P Goodman, Masoumeh Simbar, Hamid Alavi Majd, Gemma Sharp, and Fatemeh Nahidi. “The Effect of Female Genital Cosmetic and Reconstructive Procedures on Body and Genital Self-Image: A Systematic Review and Meta-Analysis.” Aesthetic Surgery Journal 43, no. 10 (September 14, 2023): 1161–73. https://doi.org/10.1093/asj/sjad109.
Asghar, Aneela, Zahid Tahir, Aisha Ghias, Usma Iftikhar, and Tahir Jameel Ahmad. “Efficacy and Safety of Intralesional Normal Saline in Atrophic Acne Scars.” Annals of King Edward Medical University 25, no. 2 (June 24, 2019). https://doi.org/10.21649/akemu.v25i2.2867.
Ashton, Leah, Hannah Nakatsuka, Colin M. Johnson, Kimberly Kenne, Karl J. Kreder, Ryan Kruse, Linder Wendt, Elizabeth B. Takacs, and Annah J. Vollstedt. “A Single Injection of Platelet-Rich Plasma Injection for the Treatment of Stress Urinary Incontinence in Females: A Randomized Placebo-Controlled Trial.” Urology, June 26, 2024, S0090-4295(24)00499-0. https://doi.org/10.1016/j.urology.2024.06.047.
Bagherani, Nooshin, and Bruce R Smoller. “Introduction of a Novel Therapeutic Option for Atrophic Acne Scars: Saline Injection Therapy.” Global Dermatology 2, no. 6 (2016). https://doi.org/10.15761/GOD.1000159.
Bernuzzi, Gino, Federica Petraglia, Martina Francesca Pedrini, Massimo De Filippo, Francesco Pogliacomi, Michele Arcangelo Verdano, and Cosimo Costantino. “Use of Platelet-Rich Plasma in the Care of Sports Injuries: Our Experience with Ultrasound-Guided Injection.” Blood Transfusion 12, no. Suppl 1 (January 2014): s229–34. https://doi.org/10.2450/2013.0293-12.
Bubnov, Rostyslav, Viacheslav Yevseenko, and Igor Semeniv. “Ultrasound Guided Injections of Platelets Rich Plasma for Muscle Injury in Professional Athletes. Comparative Study.,” n.d., 5.
Castellani, Daniele, Alessandra Valloni, Angela Piccirilli, Giuseppe Paradiso Galatioto, and Carlo Vicentini. “An Innovative Approach to Treating Vaginal Mesh Exposure after Abdominal Sacral Colpopexy: Endoscopic Resection of Mesh and Platelet-Rich Plasma; Initial Experience in Three Women.” International Urogynecology Journal 28, no. 2 (February 2017): 325–27. https://doi.org/10.1007/s00192-016-3154-x.
DeLancey, J. O. “Structural Aspects of the Extrinsic Continence Mechanism.” Obstetrics and Gynecology 72, no. 3 Pt 1 (September 1988): 296–301.
———. “Structural Support of the Urethra as It Relates to Stress Urinary Incontinence: The Hammock Hypothesis.” American Journal of Obstetrics and Gynecology 170, no. 6 (June 1994): 1713–20; discussion 1720-1723. https://doi.org/10.1016/s0002-9378(94)70346-9.
DeLong, Jeffrey M., Ryan P. Russell, and Augustus D. Mazzocca. “Platelet-Rich Plasma: The PAW Classification System.” Arthroscopy: The Journal of Arthroscopic & Related Surgery 28, no. 7 (July 2012): 998–1009. https://doi.org/10.1016/j.arthro.2012.04.148.
Dönmez, M. İrfan, Kubilay İnci, Naciye Dilara Zeybek, H. Serkan Doğan, and Ali Ergen. “The Early Histological Effects of Intravesical Instillation of Platelet-Rich Plasma in Cystitis Models.” International Neurourology Journal 20, no. 3 (September 2016): 188–96. https://doi.org/10.5213/inj.1632548.274.
Goldstein, Andrew T., Michelle King, Charles Runels, Meghan Gloth, and Richard Pfau. “Intradermal Injection of Autologous Platelet-Rich Plasma for the Treatment of Vulvar Lichen Sclerosus.” Journal of the American Academy of Dermatology 76, no. 1 (January 2017): 158–60. https://doi.org/10.1016/j.jaad.2016.07.037.
Goodman, Michael, Samantha Fashler, John R Miklos, Robert D Moore, and Lori A Brotto. “The Sexual, Psychological, and Body Image Health of Women Undergoing Elective Vulvovaginal Plastic/ Cosmetic Procedures: A Pilot Study” 28, no. 4 (2011): 9.
Graca, Flavia A., Anna Stephan, Benjamin A. Minden-Birkenmaier, Abbas Shirinifard, Yong-Dong Wang, Fabio Demontis, and Myriam Labelle. “Platelet-Derived Chemokines Promote Skeletal Muscle Regeneration by Guiding Neutrophil Recruitment to Injured Muscles.” Nature Communications 14, no. 1 (May 22, 2023): 2900. https://doi.org/10.1038/s41467-023-38624-0.
Jhang, Jia-Fong, Teng-Yi Lin, and Hann-Chorng Kuo. “Intravesical Injections of Platelet-Rich Plasma Is Effective and Safe in Treatment of Interstitial Cystitis Refractory to Conventional Treatment-A Prospective Clinical Trial.” Neurourology and Urodynamics, no. October (2018). https://doi.org/10.1002/nau.23898.
Jiang, Yuan-Hong, Yuh-Chen Kuo, Jia-Fong Jhang, Cheng-Ling Lee, Yung-Hsiang Hsu, Han-Chen Ho, and Hann-Chorng Kuo. “Repeated Intravesical Injections of Platelet-Rich Plasma Improve Symptoms and Alter Urinary Functional Proteins in Patients with Refractory Interstitial Cystitis.” Scientific Reports 10, no. 1 (September 16, 2020): 15218. https://doi.org/10.1038/s41598-020-72292-0.
Long, Cheng-Yu. “A Pilot Study: Effectiveness of Local Injection of Autologous Platelet-Rich Plasma in Treating Women with Stress Urinary Incontinence.” Scientific Reports, 2021, 9.
Matz, Ethan L, Amy M Pearlman, and Ryan P Terlecki. “Safety and Feasibility of Platelet Rich Fibrin Matrix Injections for Treatment of Common Urologic Conditions.” Investigative and Clinical Urology 59, no. 1 (January 2018): 61–65. https://doi.org/10.4111/icu.2018.59.1.61.
Middleton, Kellie K, Victor Barro, Bart Muller, Satosha Terada, and Freddie H Fu. “Evaluation of the Effects of Platelet-Rich Plasma (PRP) Therapy Involved in the Healing of Sports-Related Soft Tissue Injuries.” The Iowa Orthopaedic Journal 32 (2012): 150–63. http://www.ncbi.nlm.nih.gov/pubmed/23576936.
Moccia, Felice, Paola Pentangelo, Alessandra Ceccaroni, Antonio Raffone, Luigi Losco, and Carmine Alfano. “Injection Treatments for Vulvovaginal Atrophy of Menopause: A Systematic Review.” Aesthetic Plastic Surgery, August 14, 2023. https://doi.org/10.1007/s00266-023-03550-5.
Moraes, Vinícius Y, Mário Lenza, Marcel Jun Tamaoki, Flávio Faloppa, and João Carlos Belloti. “Platelet-Rich Therapies for Musculoskeletal Soft Tissue Injuries.” The Cochrane Database of Systematic Reviews 12 (January 2013): CD010071. https://doi.org/10.1002/14651858.CD010071.pub2.
Okumo, Takayuki, Atsushi Sato, Kanako Izukashi, Masataka Ohta, Jun Oike, Saki Yagura, Naoki Okuma, et al. “Multifactorial Comparative Analysis of Platelet-Rich Plasma and Serum Prepared Using a Commercially Available Centrifugation Kit.” Cureus 15, no. 11 (November 16, 2023). https://doi.org/10.7759/cureus.48918.
Parizzi, Natália Gomes, Oscar Ávila Rubini, Silvio Henrique Maia de Almeida, Lais Caetano Ireno, Roger Mitio Tashiro, and Victor Hugo Tolotto de Carvalho. “Effect of Platelet-Rich Plasma on Polypropylene Meshes Implanted in the Rabbit Vagina: Histological Analysis.” International Braz j Urol : Official Journal of the Brazilian Society of Urology 43, no. 4: 746–52. Accessed January 10, 2019. https://doi.org/10.1590/S1677-5538.IBJU.2016.0177.
PhD, Dr Naheed Ali, MD. “PRF vs PRP vs PRFM: The Difference and Which One Is Best.” Selphyl, August 3, 2023. https://www.selphyl.com/post/prf-vs-prp-vs-prfm-what-s-the-difference-and-which-one-is-the-best.
Pipitone, Fernanda, Zhina Sadeghi, and John O. L. DeLancey. “Urethral Function and Failure: A Review of Current Knowledge of Urethral Closure Mechanisms, How They Vary, and How They Are Affected by Life Events.” Neurourology and Urodynamics 40, no. 8 (2021): 1869–79. https://doi.org/10.1002/nau.24760.
Popp, Lothar W. “Improvement in Endoscopic Hernioplasty: Transcutaneous Aquadissection of the Musculofascial Defect and Preperitoneal Endoscopic Patch Repair.” Journal of Laparoendoscopic Surgery 1, no. 2 (January 1991): 83–90. https://doi.org/10.1089/lps.1991.1.83.
Posey, Kathleen, and Charles Runels. “In-Office Surgery and Use of Platelet Rich Plasma for Treatment of Vulvar Lichen Sclerosus to Alleviate Painful Sexual Intercourse.” Journal of Lower Genital Tract Disease 19, no. 3 (July 2015): S1–25. https://doi.org/10.1097/lgt.0000000000000121.
Prodromidou, Anastasia, Themos Grigoriadis, and Stavros Athanasiou. “Platelet Rich Plasma for the Management of Urogynecological Disorders: The Current Evidence.” Current Opinion in Obstetrics & Gynecology Publish Ahead of Print (August 18, 2022). https://doi.org/10.1097/GCO.0000000000000820.
Prodromidou, Anastasia, Dimitrios Zacharakis, Stavros Athanasiou, Athanasios Protopapas, Lina Michala, Nikolaos Kathopoulis, and Themos Grigoriadis. “The Emerging Role on the Use of Platelet-Rich Plasma Products in the Management of Urogynaecological Disorders.” Surgical Innovation, April 28, 2021, 15533506211014848. https://doi.org/10.1177/15533506211014848.
Runels, Charles. “A Pilot Study of the Effect of Localized Injections of Autologous Platelet Rich Plasma (PRP) for the Treatment of Female Sexual Dysfunction.” Journal of Women’s Health Care 03, no. 04 (2014). https://doi.org/10.4172/2167-0420.1000169.
———. “A Pilot Study of the Effect of Localized Injections of Autologous Platelet Rich Plasma (PRP) for the Treatment of Female Sexual Dysfunction.” Journal of Women’s Health Care 03, no. 04 (2014). https://doi.org/10.4172/2167-0420.1000169.
Runels, Charles, and Alexandra Runnels. “The Clitoral Injection of IncobotulinumtoxinA for the Improvement of Arousal, Orgasm & Sexual Satisfaction- A Specific Method and the Effects on Women.” Journal of Women’s Health Care 13, no. 3 No. 715 (March 20, 2024). https://doi.org/10.35248/2167-0420.24.13.715.
Sajadi, Kamran P. “Editorial Comment on ‘A Single Injection of Platelet-Rich Plasma Injection for the Treatment of Stress Urinary Incontinence in Females: A Randomized Placebo-Controlled Trial.’” Urology, July 12, 2024, S0090-4295(24)00570-3. https://doi.org/10.1016/j.urology.2024.07.013.
Saleh, Doaa M., and Rania Abdelghani. “Clinical Evaluation of Autologous Platelet Rich Plasma Injection in Postmenopausal Vulvovaginal Atrophy: A Pilot Study.” Journal of Cosmetic Dermatology n/a, no. n/a. Accessed March 9, 2022. https://doi.org/10.1111/jocd.14873.
Saltzman, Bryan M., Timothy Leroux, Maximilian A. Meyer, Bryce A. Basques, Jaskarndip Chahal, Bernard R. Bach, Adam B. Yanke, and Brian J. Cole. “The Therapeutic Effect of Intra-Articular Normal Saline Injections for Knee Osteoarthritis: A Meta-Analysis of Evidence Level 1 Studies.” The American Journal of Sports Medicine 45, no. 11 (September 1, 2017): 2647–53. https://doi.org/10.1177/0363546516680607.
Samaie Nouroozi, Atefeh, Ashraf Alyasin, Ashraf Malek Mohammadi, Nili Mehrdad, Seyed Asadollah Mossavi, Mohammad Vaezi, atoosa Gharib, Ardeshir Ghavamzadeh, and Saeed Mohammadi. “Autologous Platelet-Released Growth Factor and Sexual Dysfunction Amendment: A Pilot Clinical Trial of Successful Improvement Sexual Dysfunction after Pelvic Irradiation.” Asian Pacific Journal of Cancer Prevention 20, no. 3 (March 1, 2019): 817–23. https://doi.org/10.31557/APJCP.2019.20.3.817.
Sanoulis, Vasileios, Nikolaos Nikolettos, and Nikolaos Vlahos. “The Use of Platelet-Rich Plasma in the Gynaecological Clinical Setting. A Review.” 18, no. 3 (2019): 11.
Saraluck, Apisith, Orawee Chinthakanan, Athasit Kijmanawat, Komkrit Aimjirakul, Rujira Wattanayingcharoenchai, and Jittima Manonai. “Autologous Platelet Rich Plasma (A‐PRP) Combined with Pelvic Floor Muscle Training for the Treatment of Female Stress Urinary Incontinence (SUI): A Randomized Control Clinical Trial.” Neurourology and Urodynamics 43, no. 2 (February 2024): 342–53. https://doi.org/10.1002/nau.25365.
Sheean, Andrew J., Adam W. Anz, and James P. Bradley. “Platelet-Rich Plasma: Fundamentals and Clinical Applications.” Arthroscopy: The Journal of Arthroscopic & Related Surgery 37, no. 9 (September 2021): 2732–34. https://doi.org/10.1016/j.arthro.2021.07.003.
Toyoda, Toshihisa, Kazushige Isobe, Tetsuhiro Tsujino, Yasuo Koyata, Fumitaka Ohyagi, Taisuke Watanabe, Masayuki Nakamura, et al. “Direct Activation of Platelets by Addition of CaCl2 Leads Coagulation of Platelet-Rich Plasma.” International Journal of Implant Dentistry 4 (August 1, 2018): 23. https://doi.org/10.1186/s40729-018-0134-6.
Ural, Ülkü Mete. “The Effect of Injectable Platelet Rich Fibrin as a Nonsurgical Treatment of the Female Stress Urinary Incontinence.” Archives of Gynecology and Obstetrics 309, no. 5 (February 29, 2024): 2229–36. https://doi.org/10.1007/s00404-024-07431-3.
Zheng, Zhifang, Junfeiyang Yin, Biao Cheng, and Wenhua Huang. “Materials Selection for the Injection into Vaginal Wall for Treatment of Vaginal Atrophy.” Aesthetic Plastic Surgery 45, no. 3 (June 1, 2021): 1231–41. https://doi.org/10.1007/s00266-020-02054-w.
Tags
Platelet-rich plasma, urinary incontinence, O-Shot®, PRP injection, female stress incontinence, clinical study, placebo-controlled trial, urethra injection, patient selection, platelet activation, PRP preparation, injection technique, clitoral injection, sexual dysfunction, PRP effectiveness, gynecology, urology, PRP protocol, intravaginal injection, PRP activation, clitoral PRP, PRP studies, PRP for incontinence, vaginal wall injection, urethral injection, PRP research
Further Help
=>5-Notes Expert System for Physicians<=
=> Next Hands-On Workshops with Live Models <=
=> Dr. Runels Botulinum Blastoff Course <=
=> The Cellular Medicine Association (who we are) <=
=> Apply for Online Training for Multiple PRP Procedures <=
=> Help with Logging into Membership Websites <=
=> The software I use to send emails: ONTRAPORT (free trial) <=
|
1-888-920-5311 |
Page of |
[1] Ashton et al., “A Single Injection of Platelet-Rich Plasma Injection for the Treatment of Stress Urinary Incontinence in Females.”
[2] Sajadi, “Editorial Comment on “A Single Injection of Platelet-Rich Plasma Injection for the Treatment of Stress Urinary Incontinence in Females.”
[3] Ashton et al., “A Single Injection of Platelet-Rich Plasma Injection for the Treatment of Stress Urinary Incontinence in Females.”
[4] Long, “A Pilot Study: Effectiveness of Local Injection of Autologous Platelet-Rich Plasma in Treating Women with Stress Urinary Incontinence.”
[5] Matz, Pearlman, and Terlecki, “Safety and Feasibility of Platelet Rich Fibrin Matrix Injections for Treatment of Common Urologic Conditions.”
[6] Moccia et al., “Injection Treatments for Vulvovaginal Atrophy of Menopause.”
[7] Prodromidou, Grigoriadis, and Athanasiou, “Platelet Rich Plasma for the Management of Urogynecological Disorders.”
[8] Runels, “A Pilot Study of the Effect of Localized Injections of Autologous Platelet Rich Plasma (PRP) for the Treatment of Female Sexual Dysfunction,” 2014.
[9] Sanoulis, Nikolettos, and Vlahos, “The Use of Platelet-Rich Plasma in the Gynaecological Clinical Setting. A Review.”
[10] Dönmez et al., “The Early Histological Effects of Intravesical Instillation of Platelet-Rich Plasma in Cystitis Models.”
[11] Jhang, Lin, and Kuo, “Intravesical Injections of Platelet-Rich Plasma Is Effective and Safe in Treatment of Interstitial Cystitis Refractory to Conventional Treatment-A Prospective Clinical Trial.”
[12] Jiang et al., “Repeated Intravesical Injections of Platelet-Rich Plasma Improve Symptoms and Alter Urinary Functional Proteins in Patients with Refractory Interstitial Cystitis.”
[13] Castellani et al., “An Innovative Approach to Treating Vaginal Mesh Exposure after Abdominal Sacral Colpopexy.”
[14] Parizzi et al., “Effect of Platelet-Rich Plasma on Polypropylene Meshes Implanted in the Rabbit Vagina: Histological Analysis.”
[15] Prodromidou et al., “The Emerging Role on the Use of Platelet-Rich Plasma Products in the Management of Urogynaecological Disorders.”
[16] Saleh and Abdelghani, “Clinical Evaluation of Autologous Platelet Rich Plasma Injection in Postmenopausal Vulvovaginal Atrophy.”
[17] Samaie Nouroozi et al., “Autologous Platelet-Released Growth Factor and Sexual Dysfunction Amendment.”
[18] Zheng et al., “Materials Selection for the Injection into Vaginal Wall for Treatment of Vaginal Atrophy.”
[19] Ural, “The Effect of Injectable Platelet Rich Fibrin as a Nonsurgical Treatment of the Female Stress Urinary Incontinence.”
[20] Saraluck et al., “Autologous Platelet Rich Plasma (A‐PRP) Combined with Pelvic Floor Muscle Training for the Treatment of Female Stress Urinary Incontinence (SUI).”
[21] Runels, “A Pilot Study of the Effect of Localized Injections of Autologous Platelet Rich Plasma (PRP) for the Treatment of Female Sexual Dysfunction,” 2014.
[22] Runels and Runnels, “The Clitoral Injection of IncobotulinumtoxinA for the Improvement of Arousal, Orgasm & Sexual Satisfaction- A Specific Method and the Effects on Women.”
[23] Goldstein et al., “Intradermal Injection of Autologous Platelet-Rich Plasma for the Treatment of Vulvar Lichen Sclerosus.”
[24] Posey and Runels, “In-Office Surgery and Use of Platelet Rich Plasma for Treatment of Vulvar Lichen Sclerosus to Alleviate Painful Sexual Intercourse.”
[25] Asghar et al., “Efficacy and Safety of Intralesional Normal Saline in Atrophic Acne Scars.”
[26] Saltzman et al., “The Therapeutic Effect of Intra-Articular Normal Saline Injections for Knee Osteoarthritis.”
[27] Bagherani and R Smoller, “Introduction of a Novel Therapeutic Option for Atrophic Acne Scars.”
[28] Popp, “Improvement in Endoscopic Hernioplasty.”
[29] DeLancey, “Structural Aspects of the Extrinsic Continence Mechanism.”
[30] DeLancey, “Structural Support of the Urethra as It Relates to Stress Urinary Incontinence.”
[31] Pipitone, Sadeghi, and DeLancey, “Urethral Function and Failure.”
[32] Agarwal et al., “Comparative Efficacy of Platelet-Rich Plasma and Dry Needling for Management of Trigger Points in Masseter Muscle in Myofascial Pain Syndrome Patients.”
[33] Bernuzzi et al., “Use of Platelet-Rich Plasma in the Care of Sports Injuries.”
[34] Bubnov, Yevseenko, and Semeniv, “Ultrasound Guided Injections of Platelets Rich Plasma for Muscle Injury in Professional Athletes. Comparative Study.”
[35] Graca et al., “Platelet-Derived Chemokines Promote Skeletal Muscle Regeneration by Guiding Neutrophil Recruitment to Injured Muscles.”
[36] Middleton et al., “Evaluation of the Effects of Platelet-Rich Plasma (PRP) Therapy Involved in the Healing of Sports-Related Soft Tissue Injuries.”
[37] Moraes et al., “Platelet-Rich Therapies for Musculoskeletal Soft Tissue Injuries.”
[38] Okumo et al., “Multifactorial Comparative Analysis of Platelet-Rich Plasma and Serum Prepared Using a Commercially Available Centrifugation Kit.”
[39] DeLong, Russell, and Mazzocca, “Platelet-Rich Plasma.”
[40] Okumo et al., “Multifactorial Comparative Analysis of Platelet-Rich Plasma and Serum Prepared Using a Commercially Available Centrifugation Kit.”
[41] Toyoda et al., “Direct Activation of Platelets by Addition of CaCl2 Leads Coagulation of Platelet-Rich Plasma.”
[42] PhD, “PRF vs PRP vs PRFM.”
[43] Sheean, Anz, and Bradley, “Platelet-Rich Plasma.”
[44] Runels and Runnels, “The Clitoral Injection of IncobotulinumtoxinA for the Improvement of Arousal, Orgasm & Sexual Satisfaction- A Specific Method and the Effects on Women.”
[45] Alavi-Arjas et al., “The Effect of Female Genital Cosmetic and Reconstructive Procedures on Body and Genital Self-Image.”
[46] Goodman et al., “The Sexual, Psychological, and Body Image Health of Women Undergoing Elective Vulvovaginal Plastic/ Cosmetic Procedures: A Pilot Study.”


It’s great to see ongoing research and discussion around the effectiveness of PRP and the P-Shot® for men’s sexual health,…