When preparing platelet-rich plasma (PRP) for autologous use, sodium citrate is typically preferred over heparin for most clinical applications — particularly when the PRP is being used for tissue regeneration, aesthetic medicine, orthopedic treatments, or sexual wellness procedures.
Here’s a breakdown of when and why sodium citrate is preferred over heparin:
🔹 Use Sodium Citrate When:
-
You want to preserve platelet integrity and function
-
Sodium citrate chelates calcium and prevents clotting by reducing calcium-dependent coagulation, without directly activating platelets.
-
This maintains platelet morphology and preserves their ability to release growth factors at the injection site.
-
-
You want to avoid anticoagulants that might interfere with platelet activation
-
Heparin can affect platelet function and may inhibit some growth factor release due to interactions with proteins on platelet surfaces.
-
-
The PRP will be used for injections within a short timeframe
-
Sodium citrate is effective for keeping the sample anticoagulated for the brief period needed for PRP processing and reinjection.
-
-
The desired PRP product is leukocyte-poor (pure PRP)
-
Citrate-based systems are commonly used in aesthetic and dermatologic PRP kits that produce leukocyte-poor PRP, which is preferred in some regenerative and cosmetic procedures.
-
🔸 Use Heparin When:
-
You need to keep the plasma anticoagulated for a longer time
-
Heparin is more potent and longer-acting, useful if the PRP needs to be stored briefly or handled longer before reinjection.
-
-
The PRP will be used intraoperatively during surgery
-
In some surgical contexts, where clot formation would interfere with the procedure, heparin may be preferred.
-
-
You specifically want to prevent clotting even after reintroduction into tissues
-
This is rare in PRP use but might be considered in unique surgical or research settings.
When we perform our O-Shot®, P-Shot®, and Vampire Facelift® procedures, we want the clotting to occur soon after injection (formation of platelet-rich fibrin matrix, PRFM), so we add Calcium chloride just prior to injection. Heparin would attenuate this process and potentially decrease the effectiveness of our procedures.
-
🚫 Considerations When Using Heparin:
-
Heparin may reduce platelet aggregation and interfere with growth factor release.
-
It carries a risk of heparin-induced thrombocytopenia (HIT), even though rare in autologous settings.
-
It may alter the PRP’s biological activity, making it less ideal for regenerative applications.
✅ Summary Recommendation:
For most autologous PRP therapies intended for immediate injection into the patient, especially for aesthetic, orthopedic, sexual wellness, and wound healing applications, sodium citrate is the preferred anticoagulant due to its safety, compatibility with platelet function, and low interference with growth factor release.
⚠️ Risks Associated with Heparin
Beyond its impact on platelet function, heparin carries additional risks:
-
Heparin-Induced Thrombocytopenia (HIT)
HIT is a serious immune-mediated adverse reaction characterized by a decrease in platelet count and an increased risk of thrombosis. While rare, its occurrence necessitates caution when considering heparin for PRP preparation. Wikipedia
✅ Conclusion
Based on the evidence:
-
Sodium citrate is preferred for PRP preparation as it effectively prevents clotting without compromising platelet integrity or function.
-
Heparin, although a potent anticoagulant, can interfere with platelet activation and growth factor release, potentially reducing the regenerative efficacy of PRP.
Therefore, for autologous PRP therapies aimed at tissue regeneration, sodium citrate is the recommended anticoagulant.
ACD (Acid Citrate Dextrose) is actually a variant of sodium citrate, but it’s more refined and specifically formulated for biological applications like PRP preparation and blood banking. It’s widely regarded as superior to plain sodium citrate (TSC or trisodium citrate) for many autologous PRP applications.
🔬 Comparison: ACD vs Sodium Citrate (TSC)
| Feature | ACD-A (Acid Citrate Dextrose, Solution A) | TSC (Trisodium Citrate) |
|---|---|---|
| Mechanism | Chelates calcium to prevent coagulation | Also chelates calcium |
| Formulation | Citrate + citric acid + dextrose | Only citrate (no dextrose or acid) |
| pH stability | More stable due to buffering capacity | Less pH control |
| Platelet preservation | Excellent; minimal activation | Good but may allow more activation |
| Growth factor preservation | Better retention due to stabilized platelets | Adequate but potentially less effective |
| Osmolarity control | Balanced with dextrose for cell compatibility | Higher sodium load, less balanced |
| Usage | Preferred in many commercial PRP kits and blood banks | Also widely used in PRP preparation kits. |
✅ Advantages of ACD-A in PRP Preparation
-
Preserves Platelet Function More Effectively
-
The dextrose provides metabolic support, helping platelets maintain viability.
-
Citric acid helps stabilize pH, improving shelf-life and bioactivity.
-
-
Minimizes Premature Activation
-
ACD-A has been shown to reduce inadvertent platelet activation during processing, meaning more growth factors are available at the injection site, not lost in the tube.
-
-
Widely Used in FDA-cleared PRP Systems
-
Most commercial PRP systems (e.g., Harvest, EmCyte, Arthrex) use ACD-A for consistency and safety in autologous use.
-

⚠️ Minor Considerations
-
ACD is slightly more acidic, so some protocols recommend adding calcium chloride just before injection to re-activate platelets.
-
It may cost slightly more than plain TSC but provides greater reproducibility and bioactivity.
🟢 Bottom Line
Some think that ACD-A is generally superior to sodium citrate for autologous PRP preparation due to better platelet preservation, reduced premature activation, and more stable pH and that it is the anticoagulant of choice for high-quality, clinical-grade PRP used in orthopedics, aesthetics, sexual medicine, and regenerative therapies.
Some think that sodium citrate is superior to ACD-A.
For the past 15 years, I have used some kits with sodium citrate that work wonderfully well and some that are trash. In our membership sites, I show you my favorites based on fifteen years of experience.
What is widely acccpted: Heparin is not an appropriate anticoagulant for preparing PRP for reinjction back into the body for regenerative purposes, and is inferior to both sodium citrate and ACD-A.
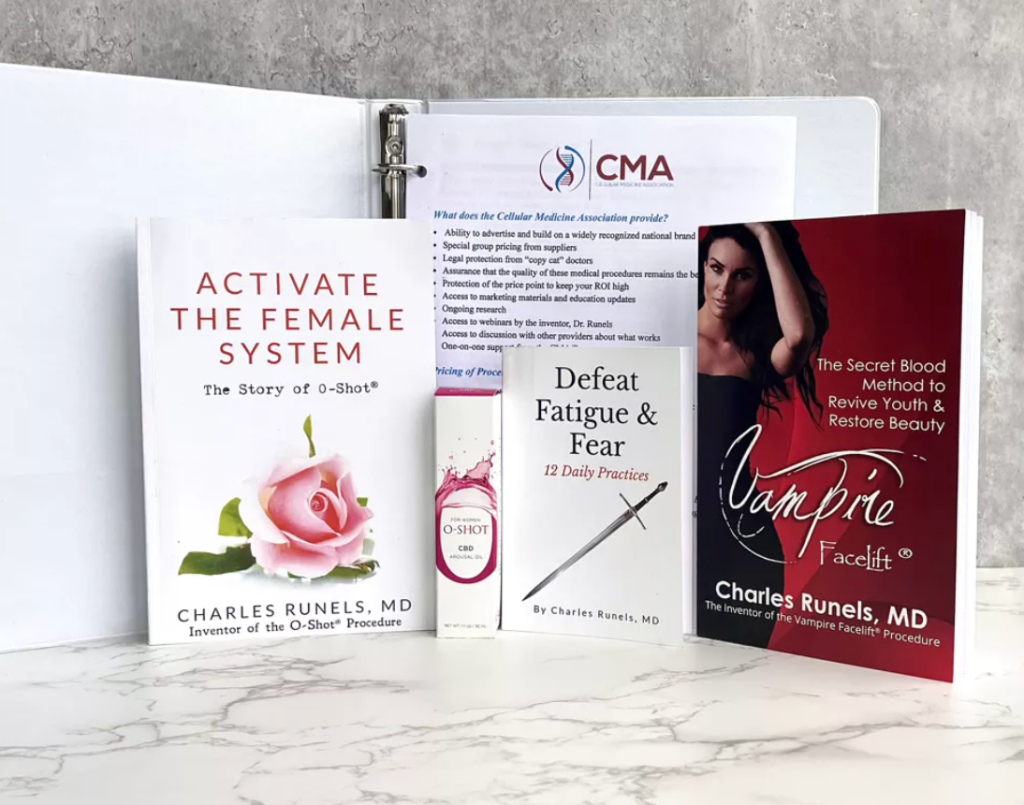
For more detailed instructions regarding best materials and practices, apply for our online and hands-on training here<–
Sincerely,
Charles Runels, MD

Cellular Medicine Association
1-888-920-5311
References
🧪 Comparative Studies on Anticoagulants in PRP Preparation
Effect of Anticoagulants on PRP Quality
A study published in the Journal of Clinical Biochemistry compared various anticoagulants used in PRP preparation. The researchers found that Acid Citrate Dextrose Solution A (ACD-A) was superior to sodium citrate (TSC) and heparin in maintaining platelet membrane integrity and preventing inadvertent activation during centrifugation. PRP produced using ACD-A released significantly more Transforming Growth Factor Beta 1 (TGF-β1) and enhanced proliferation of human marrow stromal cells compared to heparin and TSC.Impact on Mesenchymal Stromal Cells (MSCs)
Research published in Stem Cells International evaluated the effects of different anticoagulants on PRP and subsequent MSC culture. The study found that PRP obtained using sodium citrate resulted in higher platelet recovery and induced greater MSC proliferation compared to other anticoagulants. This suggests that sodium citrate is effective in preserving platelet functionality and enhancing regenerative potential.
🧬 Heparin’s Influence on Platelet Function
Heparin, while effective as an anticoagulant, can adversely affect platelet function in the context of PRP preparation:
Suppression of Platelet α-Granule Secretion
A study in the Journal of Vascular Surgery demonstrated that high concentrations of heparin suppress platelet α-granule release, which is crucial for the release of growth factors like TGF-β1 and PDGF. This suppression can diminish the therapeutic efficacy of PRP. jvascsurg.orgHeparin-Induced Platelet Activation
Research published in Blood indicated that heparin can promote platelet responsiveness by potentiating αIIbβ3-mediated outside-in signaling. This unintended activation can lead to premature degranulation of platelets, reducing the availability of growth factors at the target site. ASH Publications- McClain AK et al., 2006
Found that ACD preserved platelet integrity better than TSC and heparin, with better in vitro and in vivo performance.
(Transfusion, DOI:10.1111/j.1537-2995.2006.00918.x)- Marx RE, 2004
Described PRP preparation using ACD as the gold standard in oral/maxillofacial surgery due to better release kinetics of PDGF and TGF-β.
(Implant Dentistry, 13(4): 310–321)
Other Relevant References

It’s great to see ongoing research and discussion around the effectiveness of PRP and the P-Shot® for men’s sexual health,…